- TORCH Complex - (https://www.ncbi.nlm.nih.gov/books/NBK560528/)
About
TORCH syndrome is a medical acronym that refers to a group of congenital infections that can cause significant morbidity and mortality in newborns. This syndrome encompasses a range of infections that are transmitted from a pregnant mother to her fetus, leading to serious health issues in the infant. The acronym TORCH stands for Toxoplasmosis, Other (such as syphilis, varicella-zoster, parvovirus B19), Rubella, Cytomegalovirus (CMV), and Herpes simplex virus (HSV). These infections can result in severe developmental anomalies, organ damage, and even fetal death(1✔ ✔Trusted Source
TORCH Complex
Go to source).
Did You Know?
The risk of birth defects is highest if a woman is infected with a TORCH virus for the first time during pregnancy. This is because the developing baby's organs are still forming. #TORCH #congenitalinfections #medindiaComponents of TORCH Syndrome
Toxoplasmosis
Causative Agent: Toxoplasmosis is caused by the protozoan parasite Toxoplasma gondii
Transmission
- Maternal Infection: Usually acquired through ingestion of oocysts from contaminated food, water, or soil, or by consuming undercooked infected meat.
- Vertical Transplacental Transmission: The parasite crosses the placenta, especially during acute maternal infection.
- Fetal Impact: The parasite can infect various fetal tissues, leading to inflammation and tissue damage. The severity of damage depends on the gestational age at infection, with earlier infections causing more severe outcomes.
Clinical Manifestations
Neonatal:
- Hydrocephalus: Accumulation of cerebrospinal fluid in the brain, leading to an enlarged head.
- Chorioretinitis: Inflammation of the retina and choroid, which can cause vision problems or blindness
- Intracranial Calcifications: Abnormal calcium deposits within the brain
- Seizures: Due to neurological involvement
Long-term:
- Cognitive Impairment: Developmental delays and learning difficulties
- Vision Loss: Progressive vision impairment or blindness
- Hearing Loss: Sensorineural Hearing loss
Other Infections
Syphilis
Causative Agent: Treponema pallidum
Mechanism
- Maternal Infection: Syphilis is primarily a sexually transmitted infection. It can also be transmitted through blood transfusion or direct contact with syphilitic sores
- Transplacental Transmission: Treponema pallidum can cross the placenta at any stage of maternal infection, but transmission is more likely during primary and secondary stages of syphilis
- Fetal Impact: The spirochete bacterium can infect the fetus, causing widespread systemic infection, inflammation, and damage to multiple organs and tissues
Clinical Manifestations
- Hepatosplenomegaly: Enlarged liver and spleen.
- Jaundice: Yellowing of the skin and eyes due to liver dysfunction.
- Skin Rashes: Characteristic rash, often involving the palms and soles.
- Skeletal Abnormalities: Including periostitis, osteochondritis, and saddle nose deformity.
- Neurological Symptoms: Neurological involvement can cause developmental delays, seizures, and other nervous system abnormalities.
Varicella-Zoster Virus
Causative Agent: Varicella-zoster virus (VZV)
Mechanism
- Maternal Infection: Acquired through respiratory droplets or direct contact with vesicular lesions. Varicella (chickenpox) is highly contagious.
- Transplacental Transmission: Can occur if the mother contracts varicella during pregnancy, particularly during the first or second trimester.
- Fetal Impact: The virus causes cell death and inflammation in fetal tissues, leading to congenital varicella syndrome, which can result in a range of severe abnormalities.
Clinical Manifestations
- Skin Lesions: Scarring and limb hypoplasia (underdevelopment of limbs).
- Limb Abnormalities: Underdevelopment or deformities of limbs.
- Ocular Abnormalities: Cataracts, chorioretinitis, and microphthalmia (abnormally small eyes).
- Neurological Symptoms: Microcephaly (small head size), seizures, and developmental
- Systemic Symptoms: Low birth weight, prematurity, and potential multisystem involvement.
Parvovirus B19
Causative Agent: Parvovirus B19
Transmission
- Transplacental Infection: Parvovirus B19 can cross the placenta from an infected mother to the fetus. The virus is primarily transmitted to the mother through respiratory droplets but can also be acquired through blood transfusions.
Clinical Manifestations
Neonatal
- Fetal Anemia: Parvovirus B19 infects and destroys red blood cell precursors, leading to severe anemia in the fetus.
- Hydrops Fetalis: This is a serious condition characterized by severe edema in the fetus, resulting from heart failure due to anemia.
- Myocarditis: Inflammation of the heart muscle, which can lead to heart failure.
Rubella
Causative Agent: Rubella virus
Transmission
- Maternal Infection: Acquired through respiratory droplets from an infected person.
- Vertical Transmission: The Rubella virus can cross the placenta from an infected mother to the fetus, particularly during the first trimester of pregnancy, which poses the highest risk of severe congenital anomalies.
Clinical Manifestations
Neonatal:
- Congenital Rubella Syndrome: This syndrome includes a constellation of symptoms such as:
- Cataracts: Clouding of the lens of the eye, leading to vision impairment or blindness.
- Cardiac Defects: Including patent ductus arteriosus (PDA) and pulmonary artery stenosis.
- Sensorineural Deafness: Hearing loss due to damage to the inner ear or auditory nerve.
- Microcephaly: Abnormally small head size due to impaired brain development.
Long-term:
- Developmental Delays: Cognitive and motor delays, including difficulties with learning and coordination.
- Endocrinopathies: Increased risk of developing conditions such as diabetes mellitus and thyroid dysfunction.
Cytomegalovirus (CMV)
Causative Agent: Cytomegalovirus (CMV), a member of the herpesvirus family.
Transmission
- Maternal Infection: CMV can be transmitted through primary infection or reactivation of a latent infection. It is commonly spread through body fluids, such as saliva, urine, blood, and sexual contact.
- Vertical Transmission: CMV can be transmitted trans-placentally from an infected mother to the fetus, during delivery through contact with the birth canal, or postnatally through breast milk.
Clinical Manifestations
Neonatal
- Microcephaly: Abnormally small head size with potential for severe neurological impairment.
- Periventricular Calcifications: Calcium deposits around the brain's ventricles, indicative of brain damage.
- Hepatosplenomegaly: Enlargement of the liver and spleen.
- Jaundice: Yellowing of the skin and eyes due to liver dysfunction.
- Petechiae: Small red or purple spots on the body caused by minor bleeding under the skin.
Long-term
- Hearing Loss: Progressive sensorineural hearing loss, often detected later in childhood.
- Vision Impairment: Due to conditions such as chorioretinitis.
- Intellectual Disability: Cognitive and developmental delays.
- Motor Deficits: Issues with muscle control and coordination, potentially leading to difficulties with movement and posture.
Herpes Simplex Virus (HSV)
Causative Agent: Herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2)
Transmission
- Maternal Infection: HSV-1 typically causes oral herpes, while HSV-2 is usually associated with genital herpes. Both types can be transmitted to the neonate.
- Vertical Transmission:
- During Delivery: The most common mode of transmission, occurring when the baby comes into contact with infected genital secretions during birth.
- Transplacental Transmission: This is less common but can occur if the mother has a primary HSV infection during pregnancy.
- Postnatal Transmission: Can occur through contact with infected caregivers, usually resulting in localized skin infections.
Clinical Manifestations
Neonatal
- Skin, Eye, and Mouth Lesions (SEM Disease): Vesicular lesions on the skin, around the eyes, and in the mouth. This form of the disease is localized and less severe.
- Encephalitis: Inflammation of the brain, which can cause seizures, lethargy, irritability, poor feeding, and bulging fontanelle.
- Disseminated Infection: Involvement of multiple organs, including the liver, lungs, adrenal glands, and central nervous system. This form is the most severe and can be life-threatening.
Long-term
- Neurological Impairment: Due to encephalitis, resulting in developmental delays, intellectual disabilities, and motor deficits.
- Seizures: Chronic seizure disorders can develop as a result of brain damage.
- Recurrent Skin Lesions: Periodic reactivation of the virus can cause recurrent vesicular eruptions on the skin.
Did You Know?
Most pregnant women who are infected with a TORCH virus will not have a baby with birth defects. However, there is a risk of serious problems, such as microcephaly (a small head), intellectual disability, vision problems, hearing loss, and heart defects. #TORCHsyndrome #medindiaDiagnosis of TORCH Infections
Prenatal Diagnosis
- Ultrasound: Can detect anomalies such as hydrocephalus, microcephaly, and organomegaly and also to detect signs of fetal infection.
- Amniocentesis: To directly test for infections in the amniotic fluid.
- Maternal Serology: To determine mother’s immunity status and detect recent infections.
Neonatal Diagnosis
- Clinical Examination: To identify characteristic signs and symptoms of TORCH infections.
- Laboratory Testing: Blood tests for specific IgM antibodies, PCR for Detecting viral DNA or RNA from blood samples, and culture for bacterial infections.
- Imaging: CT or MRI to detect intracranial abnormalities and other structural defects.
Management and Treatment of TORCH Syndrome
Prenatal Management
Preventive Measures:
- Vaccination: Rubella- Ensure women of childbearing age are vaccinated against rubella prior to pregnancy.
- Avoiding Raw or Undercooked Meat: To prevent toxoplasmosis, pregnant women should avoid consuming raw or undercooked meat and practice safe handling of food.
- Good Hygiene Practices
- Handwashing: Regular handwashing, especially after handling soil, cat litter, or raw meat.
- Avoiding Contact with Infected Individuals: Pregnant women should avoid close contact with individuals known to have infections like CMV or rubella.
Maternal Treatment:
- Antimicrobial Therapy:
- Syphilis: Treated with antibiotics, typically penicillin.
- CMV: Antiviral therapy, such as ganciclovir or valganciclovir, may be considered in certain cases.
- Toxoplasmosis: Treatment with antiparasitic medications such as spiramycin or a combination of pyrimethamine and sulfadiazine with folinic acid.
Neonatal Treatment
Antibiotics and Antivirals:
- Specific Infections:
- HSV: Treated with acyclovir to reduce viral replication and manage symptoms.
- Syphilis: Treated with penicillin.
- CMV: Antiviral medications like ganciclovir or valganciclovir can be used in symptomatic neonates.
Supportive Care
- Managing Symptoms and Complications:
- Anticonvulsants: For controlling seizures, often used in cases with CNS involvement.
- Physical Therapy: For infants with motor deficits to improve muscle strength and coordination.
- Nutritional Support: Ensuring adequate nutrition, sometimes requiring specialized feeding techniques.
Follow-up
- Regular Monitoring:
- Hearing and Vision Assessments: Regular check-ups to detect and manage any sensory impairments early.
- Developmental Evaluations: Monitoring for cognitive, motor, and developmental milestones.
- Endocrine Function: Screening for conditions like diabetes mellitus in those at risk due to congenital infections.
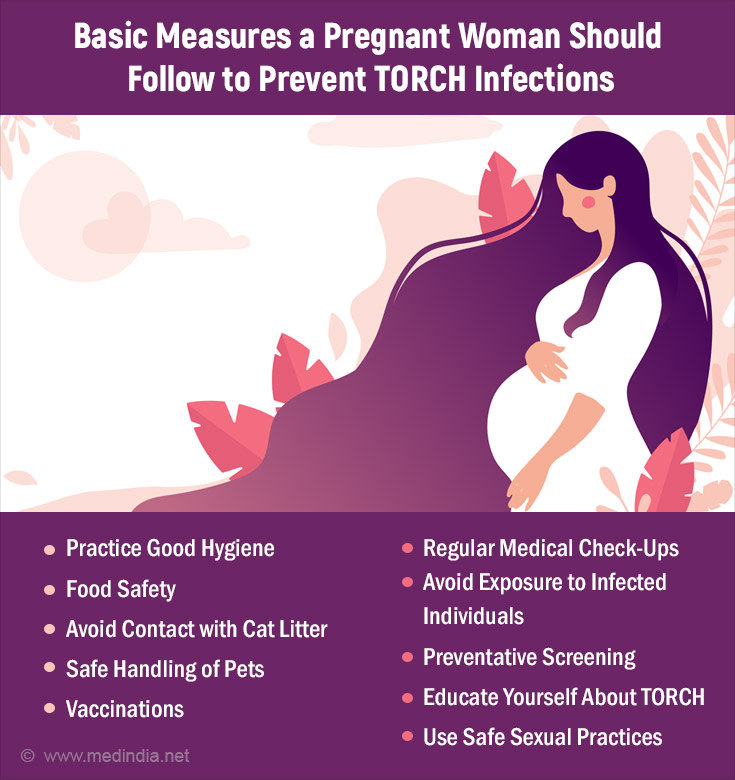
Prevention Strategies of TORCH Syndrome
Maternal Screening
- Preconception Screening: Women planning to conceive should be screened for immunity and infection status, particularly for rubella and toxoplasmosis.
- Prenatal Screening: Regular screening during pregnancy to monitor for infections such as CMV, syphilis, and HIV. Screening can include serological tests for specific antibodies (IgM and IgG) to detect recent or past infections.
- Immunizations: Women of childbearing age should receive the rubella vaccine at least one month prior to conception to ensure immunity and prevent congenital rubella syndrome.
Public Health Measures
- Education:
- Educating women about the risks of consuming raw or undercooked meat, unpasteurized dairy products, and contaminated water to prevent infections like toxoplasmosis and listeriosis.
- Promoting good hygiene practices such as regular handwashing, avoiding contact with cat litter, and not sharing eating utensils with young children to reduce the risk of CMV and other infections.
- Informing women about the risks associated with close contact with infected individuals and providing guidance on how to minimize exposure to infectious agents.
- Screening Programs:
- Implementing comprehensive screening programs for pregnant women to identify and manage infections early. This includes routine prenatal visits with serological testing and ultrasound examinations to detect any signs of fetal infection.
- Ensuring newborns are screened for signs of TORCH infections, particularly if maternal infection is suspected or confirmed. Early identification allows for prompt treatment and management of complications.
Prognosis of TORCH Syndrome
Early Diagnosis and Intervention
Early diagnosis and appropriate treatment can significantly improve outcomes for infants with TORCH infections.
Long-term Outcomes
While some infants may recover completely, others may experience long-term complications such as developmental delays, sensory impairments, and neurological deficits.
In summary, TORCH syndrome encompasses a group of infections that can lead to significant neonatal morbidity and mortality. Understanding the etiology, clinical manifestations, diagnostic approaches, and management strategies is essential for healthcare providers to ensure optimal outcomes for affected infants. Preventive measures, early diagnosis, and timely intervention are crucial components in mitigating the impact of these congenital infections.