- What is Trichotillomania (Hair Pulling Disorder)? - The TLC Foundation for Body-Focused Repetitive Behaviors - (http://www.bfrb.org/learn-about-bfrbs/trichotillomania)
- Trichotillomania - Teens Health from Nemours - (https://kidshealth.org/en/teens/trichotillomania.html)
- Trichotillomania (TTM) - OCD-UK - (https://www.ocduk.org/trichotillomania)
- Franklin ME, Zagrabbe K, Benavides KL. Trichotillomania and its treatment: a review and recommendations. Expert Rev Neurother. 2011 Aug; 11(8): 1165-74. DOI - (10.1586/ern.11.93. PMID: 21797657.)
- Christenson GA, Pyle RL, Mitchell JE. Estimated lifetime prevalence of trichotillomania in college students. J Clin Psychiatry. 1991 Oct; 52(10): 415-7. - (10.1586/ern.11.93. PMID: 21797657.)
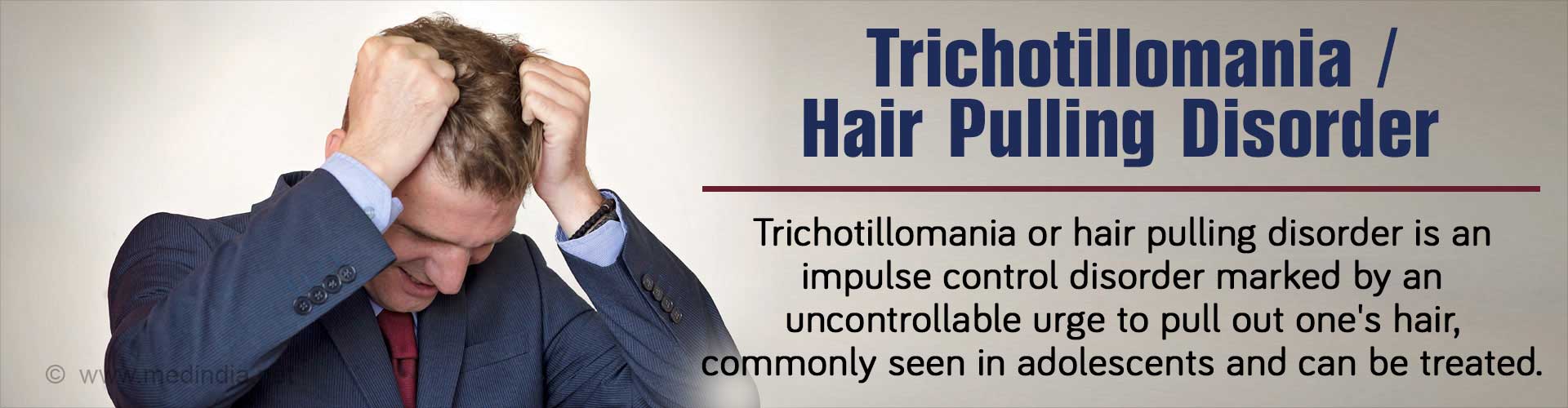
What is Trichotillomania / Hair Pulling Disorder?
Trichotillomania (TTM), commonly known as “hair pulling disorder”, is an impulse control disorder in which hair loss occurs because the patient cannot resist the urge to pull out their own hair, despite trying to stop. The most common areas affected include the scalp, eyebrows, and eyelids. This results in noticeable hair loss, clearly visible as irregular bald patches. TTM is not an obsessive-compulsive disorder (OCD) per se, but the two conditions can coexist. TTM resembles another similar condition called compulsive skin picking, technically termed as dermatillomania. TTM often runs in families, in which case a family member is more likely to be affected by the disorder.
Origin of the Term "Trichotillomania"
The term “trichotillomania” was coined by the French dermatologist François Henri Hallopeau in 1889. The name is derived from the Greek thrix (“hair”), tíllein (“to pull”), and mania (“madness”).
Epidemiology of Trichotillomania
Comprehensive, large-scale epidemiological studies for TTM are lacking. However, from smaller studies, it has been estimated that 1–3.5% of adolescents and young adults are affected by TTM. Although anecdotal evidence is available that TTM occurs in younger children, solid evidence is still lacking. Females are affected more the males.
Classification of Trichotillomania
TTM is classified in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) as an impulse control disorder. Thus, TTM falls in the same category as the obsessive-compulsive spectrum, which includes OCD, body dysmorphic disorder (BDD), nail biting (onychophagia), dermatillomania, tic disorders, and eating disorders.
However, this classification system is far from being complete and has not been unanimously accepted by all psychiatrists because of the peculiarity of the disorder. This is because TTM may seem, at times, to resemble a habit, an addiction, a tic disorder or an OCD, as a result of which a proper classification is very difficult.
What are the Causes of Trichotillomania?
TTM is undoubtedly a mental disorder, associated with changes in behavior. However, the exact cause is still unknown. Some possible causes are briefly highlighted below:
Emotional Stress: TTM can be regarded as an external manifestation of coping with mental stress, anxiety, and/or depression. This can be seen as an addiction for inflicting self-harm (hair pulling), which can provide relief from emotional distress. Importantly, TTM can overlap with the symptoms of post-traumatic stress disorder, where hair pulling has been observed.
Neurotransmitter Imbalance: TTM could result from an imbalance of chemicals (neurotransmitters) present within the brain that convey messages from one part of the brain to another part. Imbalance of neurotransmitters like serotonin and dopamine can cause changes in our mood e.g. happiness or sadness, which is often associated with TTM.
Hormonal Imbalance: It is well-established that TTM affects women more than men. Therefore, changes in the hormonal patterns in teenage girls at the time of menarche during puberty can precipitate this mental disorder.
Altered Gene Function: TTM could be caused by altered functions at the genetic level. A genetic link has been suspected for TTM, since this disorder is sometimes associated with similar disorders like OCD, which could affect the pathogenesis, disease progression, and prognosis.
Habit Formation: Since hair pulling gives a feeling of relief or satisfaction, the more the person indulges in it, the greater the urge and the stronger the habit becomes. These observations can be explained by the Neurocognitive Model, which regards TTM as a habit disorder. This stems from the fact that the basal ganglia of the brain are responsible for habit formation, while the frontal lobes are responsible for suppressing or inhibiting such habits.
What are the Symptoms & Signs of Trichotillomania?
Some of the major symptoms and signs of TTM include the following:
Intense Urge to Pull One’s Hair: Persons suffering from TTM have an intense urge to pull their hair. This can be due to a stressful condition that may act as a trigger, while it can also occur without any apparent trigger. Until and unless the person is able to pull their hair, they feel very tensed and irritable. After pulling-out the hair, the person feels a sense of pleasure, gratification, relief and/or satisfaction.
Presence of Bald Patches: Repetitive pulling of hair causes bald patches on the scalp. These can be irregular in shape, often occurring disproportionately on one side. These patches are also evident on the eyebrows, eyelashes, beard, moustache, and even the pubic and perianal areas.
Abnormal Behavior: The affected person may exhibit strange behavioral patterns pertaining to TTM. These include rituals that may accompany hair pulling and patterns of hair pulling, including preference for a certain type of hair. Others include inspecting the hair root, twirling the hair, pulling the hair between the teeth, biting, chewing, and swallowing the pulled hair. It has been demonstrated that swallowing the hair can cause gastrointestinal complications arising from trichobezoars or hairballs.
Disruption of Social Functioning: TTM causes significant disruption and impairment in social, occupational, or other important areas of functioning. This manifests as avoidance of work, school, or other public and social gatherings.
Sense of Embarrassment: Individuals suffering from TTM feel a great sense of embarrassment, often bordering upon depression. They try to conceal their bald patches from public view, often avoiding contact with anyone. They may also exhibit feelings of shame, guilt, frustration, and low self-esteem that may affect self-image, which is akin to body dysmorphic disorder.
Preference for Seclusion: Sometimes, the sufferers are so ashamed of themselves that they may prefer to live in seclusion. They avoid friends as well as any physical relationships, for fear of exposure of their condition. For the same reason, they may not even want to get married.
How do you Diagnose Trichotillomania?
Diagnosis is essentially based upon good clinical practices, such as an accurate assessment of patients in order to gather information for planning treatment and to evaluate changes in severity of symptoms.
The doctor assesses the presenting symptoms, severity of the symptoms, functional impairment (if any), differential diagnosis, and comorbidities.
Briefly, a diagnosis of trichotillomania can be considered if the following are present
- Repeated hair pulling results in noticeable hair loss
- Feeling of anxiety or distress just before pulling out the hair or trying to resist the behavior
- Sense of relief and pleasure when pulling out the hair
- No other obvious mental or medical condition found to explain the symptoms
- Socially impacts the life of the person
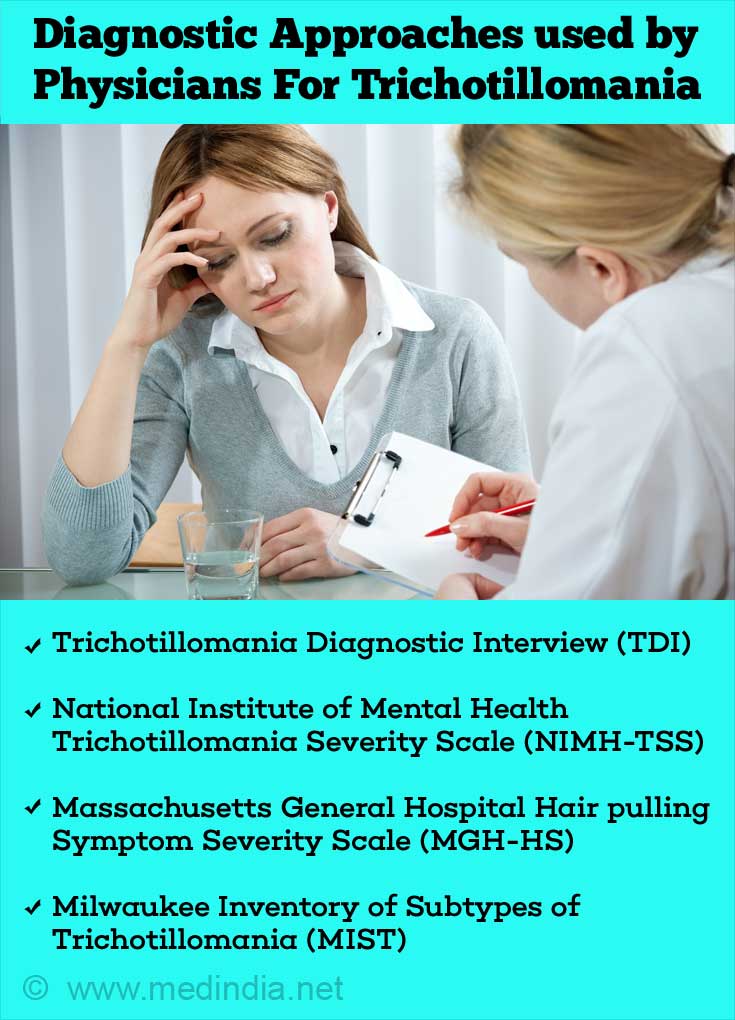
There are several diagnostic approaches that are currently used to diagnose and evaluate the condition of patients suffering from TTM. All these are based upon a set of questionnaires that are given to the patients to fill-up. These questionnaires are aimed at assessing the mental state of the patients with reference to the disorder. Based upon the patients’ responses, the doctor makes a diagnosis. Besides these questionnaires, photographic evidence is also gathered. These diagnostic approaches are listed below:
- Trichotillomania Diagnostic Interview (TDI)
- National Institute of Mental Health Trichotillomania Severity Scale (NIMH-TSS)
- Massachusetts General Hospital Hair pulling Symptom Severity Scale (MGH-HS)
- Milwaukee Inventory of Subtypes of Trichotillomania (MIST)
- Premonitory Urge Scale (PUS) or Premonitory Urge for Tics Scale (PUTS)
- Photography: Photographs are taken not only for diagnostic purposes, but also to monitor the progression of treatment. Photographs are generally taken of the patients’ primary pulling sites and the bald areas.
How do you Treat Trichotillomania?
There are a wide variety of treatment options for TTM that are currently available for children, adolescents and adults. These include cognitive behavioural therapy (CBT), counselling, support groups, hypnosis, pharmacotherapy, and combined approaches. Some of the major strategies for the treatment of TTM are briefly discussed below:
Cognitive Behavioral Therapy (CBT): CBT is a three-pronged approach:
- Awareness Training: This uses techniques that make the patient aware of his/her condition by way of self-monitoring. For example, maintaining a diary where the patient records the number of urges he/she experiences.
- Impulse Control: This aims at finding out the triggers that cause hair pulling and learning how to avoid them.
- Competing Response Training: Also known as habit-reversal training, this involves teaching the patient to replace hair pulling with a physically incompatible behavior, like squeezing a stress ball.
Pharmacotherapy: This approach uses medicines to treat TTM. Some of these pharmacological molecules are briefly highlighted below:
- Selective Serotonin Reuptake Inhibitors (SSRI): These drugs are typically used as antidepressants to treat anxiety disorders and major depression. However, it is now generally accepted that SSRIs are not considered as first-line therapy for TTM per se. However, combination therapy with SSRI and CBT has been found to be superior to SSRI or CBT alone.
- Clomipramine: This is a tricyclic antidepressant with serotonergic and other properties that has been found to be efficacious for treating TTM. However, due to its unfavorable side-effects, it has been relegated to a second-line therapy for TTM.
- New Pharmacological Agents: Recent research has revealed the efficacy of three new pharmacologic agents for the treatment of TTM. These include an opioid antagonist (naltrexone), a glutamate modulator (N-acetylcysteine [NAC]) and an atypical neuroleptic (olanzapine).

What are the Complications of Trichotillomania?
There may be several complications arising from TTM. These are briefly highlighted below:
Decreased Quality of Life: The quality of life can become decreased substantially, because the patient is always bogged down by feelings of guilt, shame, isolation, and embarrassment. This greatly hampers social functioning, such as absenteeism from school/work, fewer friends, and difficulty in intimate relationships. Many of the sufferers become frustrated and angry in not being able to control their urges, which often leads to substance abuse, such as alcohol, smoking, and drug abuse. Importantly, this situation is a vicious circle, escape from which is very difficult.
Traction Alopecia: Alopecia means hair loss. TTM results in extensive hair loss due to constantly pulling-out the hair, in which case it is termed as traction alopecia. This causes bald patches on the scalp, which leads to substantially reduced self-confidence and self-esteem.
Trichobezoars: These are hair balls that can form in the stomach or intestine as a result of eating the pulled hair. This can cause serious problems such as peptic perforation, obstructive jaundice, and acute pancreatitis. In severe cases, surgery may be required to remove the trichobezoars.
Psychiatric Complications: Psychiatric complications are common sequelae of TTM. These include anxiety disorders, mood disorders, substance abuse disorders, eating disorders and personality disorders. In case of teenagers, disruptive behavior disorders are the most prominent complications.