- Type 3c (Pancreatogenic) Diabetes - (https://en.wikipedia.org/wiki/type_3c_(pancreatogenic)_diabetes)
- Anatomy and Histology of the Pancreas - (https://www.pancreapedia.org/reviews/pancreatogenic-type-3c-diabetes)
- Pancreatogenic (Type 3c) Diabetes - (https://www.pancreapedia.org/reviews/anatomy-and-histology-of-pancreas)
- Pancreas: Anatomy and Functions - (https://www.hopkinsmedicine.org/healthlibrary/conditions/liver_biliary_and_pancreatic_disorders/pancreas_anatomy_and_functions_85,p00682)
- Management of pancreatogenic diabetes: challenges and solutions - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc5003514/)
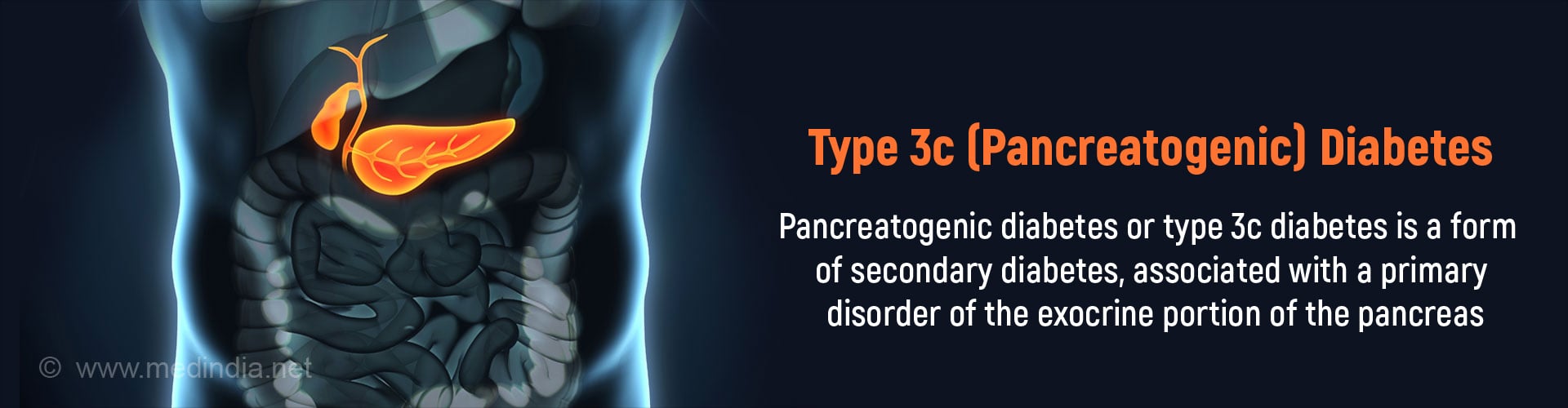
What is Type 3c (Pancreatogenic) Diabetes?
Pancreatogenic or type 3c diabetes mellitus is a form of secondary diabetes wherein the primary disease is in the exocrine portion of the pancreas and predates the development of diabetes.
It is suggested that between 5-10% of all diabetics may have pancreatogenic diabetes.
Interestingly nearly 80 percent of pancreatogenic diabetes is caused by chronic pancreatitis. The exact figures are not known as data remains scarce and frequently patients with pancreatic diabetes are misclassified.
Only recently have diagnostic criteria been proposed for pancreatogenic diabetes, enabling accurate diagnosis and appropriate management of the condition.
Pancreas - Overview of Structure and Function
The pancreas is an important organ found in the abdominal cavity. It is elongated and tapering and is situated behind the stomach. The pancreas is structurally divided into four parts namely head, neck body and tail.
Functionally, it is divided into two portions, the exocrine portion and the endocrine portion.
- The exocrine portion occurs predominantly in the head, neck and body and consists of glands that secrete digestive juices which travel to the small intestine through ducts. The secretions of the exocrine pancreas are essential for the breakdown of carbohydrates, proteins and fats into smaller molecules in the small intestine which are then absorbed into the bloodstream.
- The endocrine portion of the pancreas, also referred to as the islets of Langerhans is distributed throughout the pancreatic tissue. Some studies suggest that the highest density of islet cells is found in the tail portion of the pancreas. Overall, the islet cells comprise only 1-2% of the adult pancreatic tissue.
The endocrine portion of the pancreas (islets) secretes two important hormones directly into the bloodstream, namely insulin and glucagon. Both these hormones are important in carbohydrate metabolism and regulation of blood sugar levels.
Thus the pancreas is an important organ and diseases of the pancreas can have a serious impact on the health of an individual.
Common Diseases of the Pancreas
- Diseases affecting the exocrine pancreas include acute and chronic pancreatitis due to various causes, cancer, trauma, cystic fibrosis, and hemochromatosis.
- The most common disease of the endocrine pancreas is diabetes mellitus wherein there is an absolute or relative deficiency of insulin hormone. Due to insulin deficiency, glucose is not metabolised properly resulting in increased blood glucose levels (hyperglycemia).
Types of Diabetes Mellitus
There are two main types of diabetes mellitus caused when the endocrine pancreas is affected.
Type 1 diabetes occurs when the insulin secreting cells (beta cells) in the islets are attacked by the body's immune system and destroyed. This results in absolute insulin deficiency.
In type 2 diabetes, the body becomes unresponsive and resistant to the effects of the insulin hormone. As a result more insulin needs to be released by the pancreas to bring down blood glucose levels. Over time the capacity of the beta cells to produce insulin is diminished.
A rare form of diabetes called pancreatic diabetes occurs when the disorder is primarily in the exocrine pancreas which predates the development of diabetes. It is also referred to as Type 3c diabetes. It is therefore a form of secondary diabetes because the primary pathology is NOT in the endocrine pancreas.
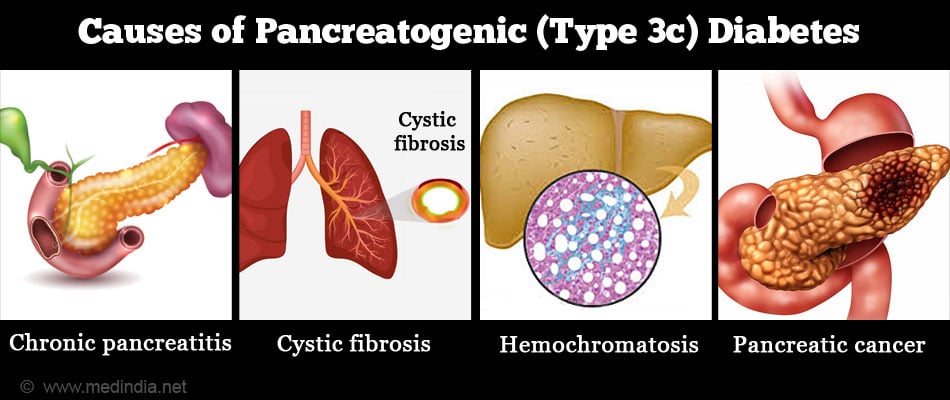
What are the Causes of Type 3c (Pancreatogenic) Diabetes?
Several disorders of the exocrine pancreas can cause pancreatogenic (type 3c) diabetes.
These include the following:
- Chronic pancreatitis - The most important cause accounting for nearly 80% of cases. The risk of developing type 3c diabetes in chronic pancreatitis increases with duration and severity of the pancreatitis. Surgical resection, especially of the distal pancreas accelerates the development of type 3c diabetes
- Acute pancreatitis - Sudden inflammation of the exocrine pancreas mainly due to alcohol abuse and gallstones
- Relapsing pancreatitis - Recurrent episodes of pancreatitis
- Cystic fibrosis - An inherited disorder which causes inflammation and progressive scarring of the exocrine pancreatic glands due to blockage of the pancreatic ducts by mucus plugs
- Hemochromatosis - Another inherited disorder characterized by iron overload in the body, including the pancreas leading to destruction of the exocrine glands
- Pancreatic cancer
- Pancreatectomy - Surgical removal of pancreas for example, in cancer
- Pancreatic agenesis - Absent or defective development of pancreas
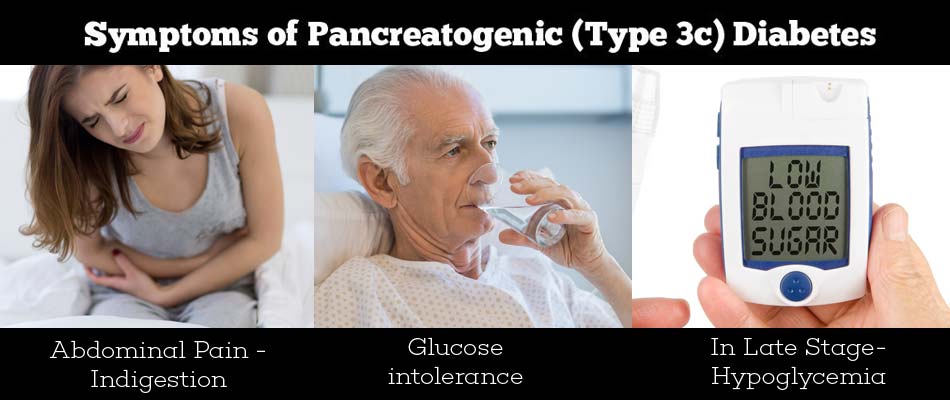
What are the Symptoms of Type 3c (Pancreatogenic) Diabetes?
Most patients with pancreatogenic type 3c diabetes have a history of chronic pancreatitis with exocrine pancreatic insufficiency characterized by abdominal pain, steatorrhea (increased fat in stools which float) or impaired digestion with nutritional deficiencies and glucose intolerance when there is endocrine involvement.
Some cases present with abdominal pain and indigestion without a history of pancreatitis.
Occasionally, only glucose intolerance may be evident with no features of pancreatic disease.
In later stages of the disease, with progressive loss of islet cells and decreased glucagon secretion as well, there may be frequent attacks of hypoglycemia (low blood sugar levels).
How do you Diagnose Type 3c (Pancreatogenic) Diabetes?
To improve the diagnosis of type 3c diabetes and reduce wrong misclassification of patients, Ewald and Bretzel proposed diagnostic criteria which include major and minor criteria. To make a diagnosis of type 3c diabetes, all three major criteria MUST be present.
- Occurrence of exocrine pancreatic insufficiency (according to monoclonal fecal elastase-1 or direct function tests)
- Pancreatic imaging such as MRI, CT or endoscopic ultrasound that reveals pancreatic disease
- Absence of autoimmune markers associated with type 1 diabetes (autoantibodies)
The major criteria may be further supported by the presence of additional minor criteria such as
- Impaired beta cell function, as measured by the oral glucose tolerance test (OGTT). A diagnosis of diabetes is made by a two-hour blood glucose level ≥200 mg/dl, and impaired glucose tolerance is said to occur when a two-hour glucose measures 140-199 mg/dl, also consistent with pre-diabetes
- No evidence for presence of insulin resistance as measured for example, by Homeostatic Model Assessment of Insulin Resistance (HOMA-IR)
- Low serum levels of lipid soluble vitamins A,D,E and K (since fat digestion is impaired in exocrine pancreatic insufficiency)
- Impaired incretin secretion (which normally stimulates insulin secretion, for example, gastric inhibitory polypeptide or pancreatic polypeptide secretion, normally secreted by the islet cells
How do you Treat Type 3c (Pancreatogenic) Diabetes?
The primary target for the management of type 3c diabetes as with type 1 and type 2 remains control of hyperglycemia to achieve and maintain the HbA1c <7%, in order to minimize the risk of heart, kidney, eye and nerve related complications.
The various forms of management include:
- Lifestyle modifications to reduce risk of pancreatic diabetes and to prevent associated complications
- Nutritional support
- Medications
- Surgery
Lifestyle modifications:
Quit smoking and alcohol since these contribute to increased inflammation of the pancreas and fibrosis. Maintain healthy weight since obesity decreases insulin sensitivity.
Nutritional Support
The chief aim of medical nutritional therapy in chronic pancreatitis-associated diabetes include the following:
- Preventing and / or treating malnutrition by urging patients to eat meals rich in soluble fiber and low in fat
- Control of symptoms of steatorrhea with pancreatic enzyme supplements
- Reduce hyperglycemia following meals
- Oral enzyme replacement therapy for exocrine pancreatic insufficiency. Enzyme replacement is particularly important to aid fat digestion and absorption of nutrients absorption, and also prevent fat-soluble vitamin deficiency. It also maintains incretin hormone secretion, thereby improving glucose tolerance
- Treating associated Vitamin D deficiency frequently present in chronic pancreatitis with supplements
In cystic fibrosis-related pancreatogenic diabetes (CFRD), the goals of therapy include:
- Achieving optimal nutritional status and normal blood glucose levels
- Consuming a well-balanced diet with no restriction in caloric intake, and no carbohydrate or fat restriction
- Supplementation of fat soluble vitamins
Unlike other types of diabetes, salt and protein restriction is not recommended in CFRD, even in the background of arterial hypertension or microvessel complications.
Antihyperglycemic agents:
In chronic pancreatitis that is associated with mild diabetes, an oral antihyperglycemic agent, such as metformin, which improves insulin sensitivity may be considered. Oral anti-hyperglycemic agents are not useful in CFRD, as they are less effective than insulin in improving the metabolic or nutritional status of the patient.
Treatment with insulin is preferred in most patients, especially to correct hyperglycemia in CFRD, for severely malnourished, acutely ill or hospitalized patients, wherein the metabolic effects of insulin are especially beneficial for the patient.
Surgery:
Total pancreatectomy with islet autotransplantation is a surgical method employed in select patients to treat severe complications such as pain of recurrent acute and chronic pancreatitis with frequent hospitalizations, reducing the risk of severe diabetes mellitus and in persons with a high risk of pancreatic cancer.
Promising New Drugs
One of the emerging drugs that have shown great promise in the treatment of type 3c diabetes, secondary to chronic pancreatitis is pancreatic polypeptide (PP). It increases the expression of insulin receptors in the liver, thereby allowing better and more effective utilization of circulating insulin. It also enhances insulin sensitivity and reduces insulin requirements in type 3c diabetes patients.
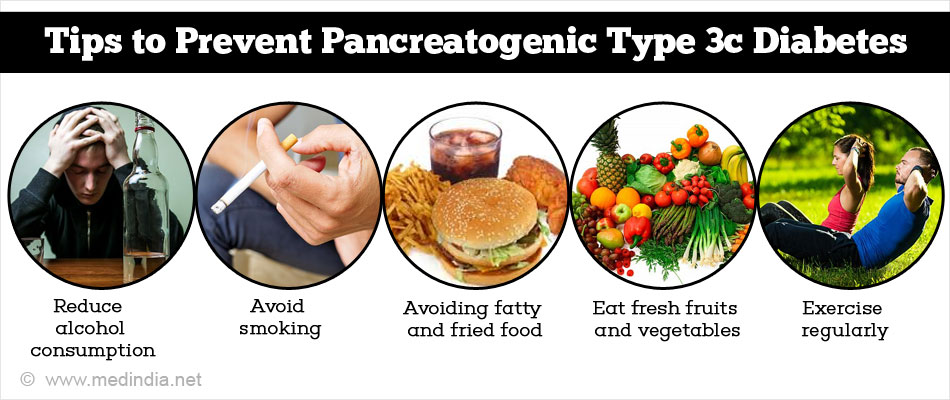
How do you Prevent Type 3c (Pancreatogenic) Diabetes?
Pancreatogenic type 3c diabetes due to chronic pancreatitis may be prevented by reducing the risk factors of developing chronic pancreatitis. These include the following:
- Reduce alcohol consumption
- Avoid smoking
- Reduce chances of developing gallstones by avoiding fatty and fried foodstuffs and maintaining a healthy weight
- Eat a healthy diet rich in fresh fruits and vegetables
- Exercise regularly and avoid obesity