- Dermatomyositis - (https://www.ncbi.nlm.nih.gov/books/NBK558917/)
About
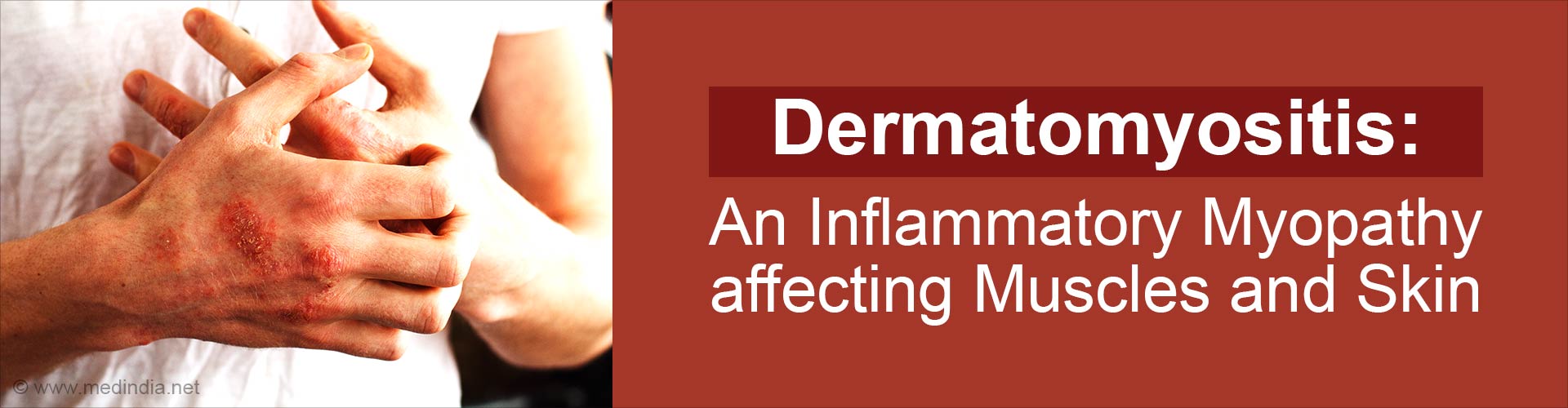
Dermatomyositis belongs to a group of diseases known as inflammatory myopathies. It affects the muscles and skin, causing muscle weakness and skin rashes. It mainly affects muscles used for moving and the skin, causing different symptoms in each person(1✔ ✔Trusted Source
Dermatomyositis
Go to source).
Did You Know?
Dermatomyositis is diagnosed more frequently in Women than Men.Types of Dermatomyositis
- Classic Dermatomyositis: This subtype typically manifests with proximal muscle weakness, meaning weakness in muscles closest to the trunk of the body. Patients often experience difficulty in climbing stairs, rising from a seated position, or lifting objects. The characteristic skin rash, known as heliotrope rash, appears as a purplish discoloration around the eyelids, often accompanied by swelling.
- Amyopathic Dermatomyositis: Unlike classic dermatomyositis, this variant primarily affects the skin without significant muscle involvement. The absence of muscle weakness can make diagnosis challenging, as patients may present solely with skin manifestations such as Gottron's papules (raised, scaly patches on the knuckles).
- Juvenile Dermatomyositis: This form primarily affects children, with symptoms varying in severity. In addition to muscle weakness and skin rashes, children may experience complications such as calcinosis (calcium deposits in the skin and muscles), which can lead to joint stiffness and pain.
- Overlap Syndrome: Dermatomyositis may coexist with other autoimmune diseases such as systemic lupus erythematosus or scleroderma, leading to a more complex clinical picture. Overlap syndromes often require tailored treatment approaches addressing multiple autoimmune processes simultaneously.
Causes of Dermatomyositis
Multifactorial Etiology: Dermatomyositis is believed to result from a complex interaction of genetic, environmental, and immunological factors.
Genetic Predisposition: Certain genetic variants may predispose individuals to develop dermatomyositis. However, the exact genes involved and their mechanisms of action remain incompletely understood.
Environmental Triggers: Various environmental factors have been implicated in triggering or exacerbating dermatomyositis. These include:
Viral Infections: Viruses such as coxsackievirus and parvovirus have been associated with the onset or worsening of dermatomyositis. The viral infection may stimulate an abnormal immune response, leading to inflammation and tissue damage.
Medications: Certain medications, particularly statins (used to lower cholesterol), have been linked to the development of dermatomyositis. It is hypothesized that these drugs may trigger an autoimmune reaction in susceptible individuals.
Ultraviolet Radiation: Exposure to ultraviolet (UV) radiation from sunlight or artificial sources may exacerbate skin manifestations in dermatomyositis patients. UV radiation can induce inflammation and oxidative stress in the skin, aggravating existing lesions and promoting disease progression.
Immune Dysregulation: Dysregulation of the immune system is a central feature of dermatomyositis pathogenesis. Aberrant activation of immune cells, including T lymphocytes and B lymphocytes, leads to the production of autoantibodies and pro-inflammatory cytokines. These immune mediators contribute to tissue damage and inflammation in affected muscles and skin.
Complex Interplay: The development of dermatomyositis likely involves a complex interplay between genetic susceptibility, environmental triggers, and dysregulated immune responses. Elucidating the precise mechanisms underlying these interactions remains an ongoing area of research in the field of autoimmune disorders.
Symptoms and Signs of Dermatomyositis
Beyond the hallmark features of muscle weakness and skin rash, dermatomyositis can present with a spectrum of systemic manifestations. These include:
Skin Involvement: Dermatomyositis exerts a profound impact on the integumentary system, affecting not only the epidermis but also dermal structures such as sweat glands and hair follicles. Cutaneous manifestations may extend beyond the characteristic rash to include photosensitivity, alopecia (hair loss), and ulcerations, further complicating disease management.
Dysphagia (Difficulty Swallowing): Muscle weakness in the throat (pharyngeal muscles) and esophagus can lead to dysphagia, making it challenging for individuals with dermatomyositis to swallow food and liquids. Dysphagia can result in aspiration (food or liquid entering the airway), which may lead to complications such as pneumonia or malnutrition if not properly managed.
Interstitial Lung Disease (ILD): Dermatomyositis-associated ILD is a common pulmonary complication characterized by inflammation and scarring of the lung tissue. Patients may experience symptoms such as cough, shortness of breath, and exercise intolerance. ILD can progress to respiratory failure if left untreated, highlighting the importance of regular pulmonary function testing and early intervention.
Cardiac Involvement: Dermatomyositis can affect the heart, leading to various cardiac manifestations. These may include arrhythmias (irregular heart rhythms), myocarditis (inflammation of the heart muscle), and congestive heart failure. Cardiac involvement in dermatomyositis can significantly impact prognosis and may require specialized cardiac monitoring and management.
Gastrointestinal Involvement: In addition to Dysphagia, dermatomyositis can affect the gastrointestinal tract, leading to symptoms such as abdominal pain, diarrhea, and weight loss Gastrointestinal complications may result from muscle weakness affecting the smooth muscle of the digestive system or from systemic inflammation associated with the disease.
Joint Pain and Arthritis: Some individuals with dermatomyositis may experience joint pain and arthritis, characterized by inflammation and stiffness of the joints. Joint involvement can vary in severity and may mimic other rheumatic conditions such as rheumatoid arthritis. Proper diagnosis and management of joint symptoms are essential for optimizing patient outcomes.
Vascular Abnormalities: Dermatomyositis can be associated with vascular abnormalities such as vasculitis (inflammation of blood vessels) and Raynaud's phenomenon (vasospasm of small arteries in response to cold or stress). These vascular manifestations may lead to skin ulcers, digital ischemia (reduced blood flow to the fingers or toes), and other complications requiring specialized vascular assessment and treatment.
Did You Know?
Dermatomyositis, though considered rare, can significantly impact various organs beyond muscles and skin, including the lungs, heart, and gastrointestinal tract.Treatments for Dermatomyositis
Mitigating Symptoms and Suppressing Inflammation:
- Treatment goals in dermatomyositis focus on alleviating symptoms and controlling inflammation to prevent disease progression and complications.
- Corticosteroids, such as prednisone or prednisolone, are commonly used as first-line therapy to suppress immune-mediated inflammation and induce remission of disease activity.
- High doses of corticosteroids may be initiated initially and gradually tapered down to the lowest effective dose to maintain disease control while minimizing long-term side effects.
Immunosuppressive Agents:
- In cases where corticosteroids alone are insufficient to achieve disease control or to minimize long-term steroid dependence, immunosuppressive agents are often prescribed as steroid-sparing agents.
- Methotrexate, azathioprine, mycophenolate mofetil, and rituximab are among the immunosuppressive medications commonly used in dermatomyositis treatment.
- These agents work by modulating the immune response and reducing inflammation, thereby helping to preserve muscle function and prevent disease flare-ups.
Physical and Occupational Therapy:
- Physical and occupational therapy are integral components of dermatomyositis management, aimed at maintaining muscle strength, improving mobility, and enhancing overall quality of life.
- Physical therapy focuses on exercises and rehabilitation techniques designed to strengthen weakened muscles, improve range of motion, and alleviate pain and stiffness.
- Occupational therapy addresses functional limitations and helps patients develop adaptive strategies to perform activities of daily living more independently.

Sun Protection:
- Sun protection measures are essential for individuals with dermatomyositis, as increased sensitivity to ultraviolet (UV) radiation can exacerbate skin manifestations and trigger disease flares.
- Patients are advised to minimize sun exposure, wear protective clothing, and use broad-spectrum sunscreen with a high sun protection factor (SPF) when outdoors.
Monitoring and Follow-Up:
- Regular monitoring and follow-up are essential components of dermatomyositis care to assess disease activity, monitor treatment response, and detect potential complications.
- Laboratory tests, including muscle enzyme levels (e.g., creatine kinase), inflammatory markers (e.g., erythrocyte sedimentation rate), and autoantibody testing, may be performed periodically to evaluate disease activity and treatment efficacy.
Multidisciplinary Approach:
- Dermatomyositis management often requires a multidisciplinary team approach involving rheumatologists, dermatologists, neurologists, pulmonologists, physical therapists, occupational therapists, and other healthcare professionals.
- Collaboration among specialists ensures comprehensive care tailored to the individual needs of patients and facilitates the timely implementation of therapeutic interventions and supportive services.
Conclusion
Although considered rare, dermatomyositis warrants increased recognition and research efforts to elucidate its pathogenesis and optimize therapeutic interventions. Collaborative initiatives among clinicians, scientists, and patient advocacy groups are essential in advancing scientific understanding and improving outcomes for individuals afflicted by this complex autoimmune disorder.
Dermatomyositis epitomizes the intricate interplay between immune dysregulation and tissue-specific autoimmunity, necessitating a comprehensive approach to diagnosis, treatment, and ongoing management. By elucidating the underlying mechanisms driving disease pathogenesis and leveraging innovative therapeutic modalities, clinicians and researchers can strive towards enhancing the prognosis and quality of life for individuals living with dermatomyositis.