- What is Continuous Glucose Monitoring? - (https://www.medtronic-diabetes.in/products/continuous-glucose-monitoring)
- Blood sugar testing: Why, when and how - (https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/blood-sugar/art-20046628)
- All About Continuous Glucose Monitors for People with Diabetes - (https://www.uabmedicine.org/-/all-about-continuous-glucose-monitors-for-people-with-diabetes)
- Continuous Glucose Monitoring - (https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes/continuous-glucose-monitoring)
- About Continuous Glucose Monitoring - (https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/testing/continuous-glucose-monitoring-cgm)
- Information About Continuous Glucose Monitoring - (https://my.clevelandclinic.org/health/drugs/11444-glucose-continuous-glucose-monitoring)
Overview
Diabetes (be it Type 1 or Type 2) — a metabolic condition characterized by abnormally higher blood glucose (sugar) levels is becoming a grave problem worldwide. It is estimated to affect 30.3 million (1 in 10) Americans as per the Centers for Disease Control & Prevention.
Generally, blood glucose is managed by diet, medication, and exercise by monitoring the blood glucose through the traditional finger-prick method or laboratory testing. The revolution of technology also emanates a more convenient and less painful way to keep the blood glucose levels in check — continuous glucose monitors (CGMs).
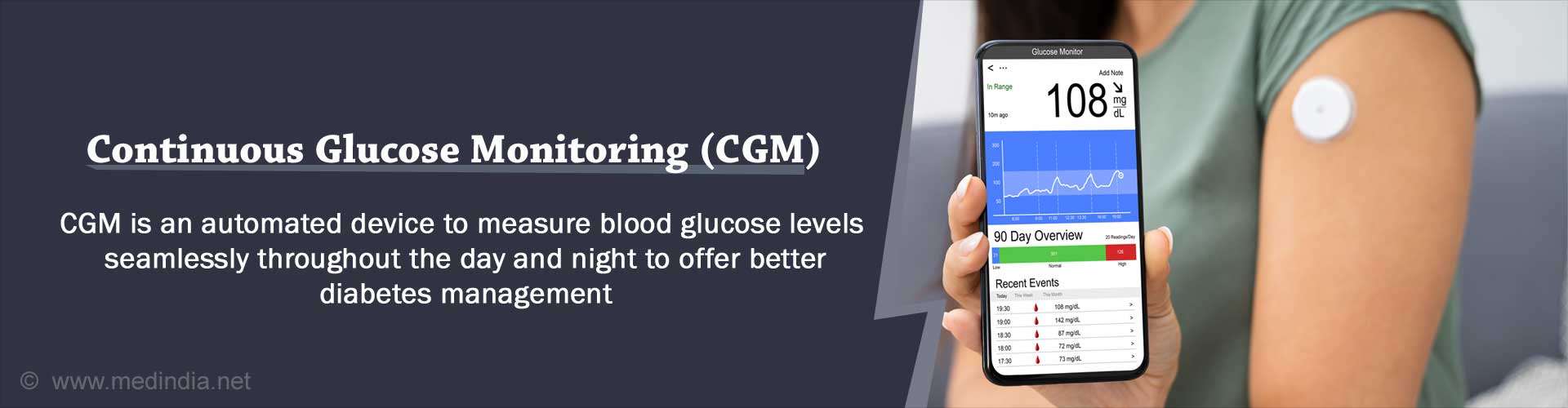
What is Continuous Glucose Monitor (CGM)?
A CGM is an automatic measuring device for blood glucose levels throughout the day and night. This offers glancing at the trends of your sugar levels at any point in time — over a few hours or days.
The first continuous glucose monitoring system among diabetic patients for use at home was approved by the U.S. Food & Drug Administration was in 1991. The monitor utilizes the glucose levels in the interstitial fluid (surrounding the blood vessels) to measure the blood glucose.
The CGM involves placing a sensor beneath the skin to measure the 24 hours glucose levels and simultaneously warn one about critically high or low blood glucose levels. The results are traceable from a wearable device or cell phone, which is sent via the transmitter.
This easy approach may help individuals take real-time positive lifestyle decisions to monitor the body’s glucose changes through medicines, food, and physical activity.
How Does a Continuous Glucose Monitor Work?
A CGM works by wirelessly measuring your interstitial glucose level (fluid between the cells). The sensor records the blood glucose levels at almost any time — when you are working, sleeping, showering, or even exercising. An alarm is typically enabled to indicate too high or too low glucose levels.
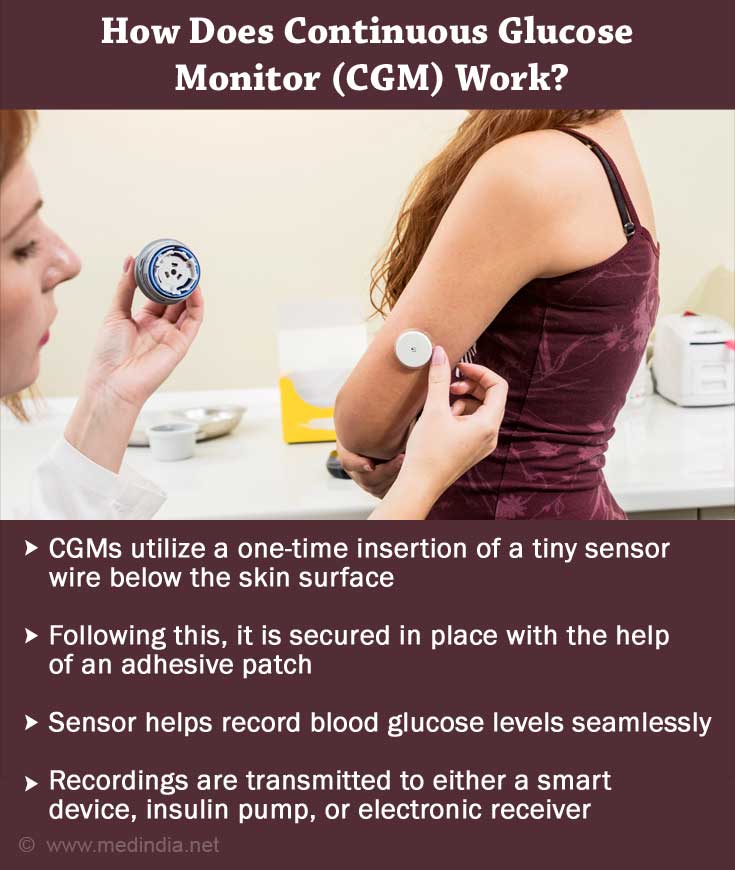
Unlike traditional glucose monitors (that require multiple fingertips prick to test the blood glucose), CGMs utilize a one-time insertion of a tiny sensor wire below the skin surface of the abdomen (belly) or the arm’s back. Following this, it is secured in place with the help of an adhesive patch for continuous recording of the blood glucose levels.
The glucose readings are recorded by the sensor from the interstitial fluid beneath your skin every five minutes and are then transmitted to either a smart device, insulin pump, or electronic receiver. This helps chart down the real-time glucose data of the users and can also be downloaded to a computer seamlessly.
Some of the CGM models are recommended for use among people above the age of 18 years. However, there are models available for use in children as young as the age of 2 years.
Among several models of CGM devices listed by the American Diabetes Association, the current ones can be worn for continuous 7 to 14 days. However, the long-term CGM models available for implantation require a change of the sensor by the healthcare provider.
Things to Remember When Using a CGM
- If you are using a CGM for the first time, it is important to calibrate the devicewith the help of your professional or by measuring the blood glucose levels on a standard glucose meter twice a day (both the CGM and standard reading should be matching).
- Any person with type 1 or type 2 diabetes can use a CGM for real-time blood glucose monitoring.
- Depending on various models, one may also have to replace the CGM sensoronce every 3 to 7 days.
- It is important to undertake necessary actions on a CGM alarm sound (towards critical levels of blood glucose) or consult your diabetologist
What are the Benefits of a CGM?
Some of the benefits of CGM, when compared to a standard blood glucose meter, are:
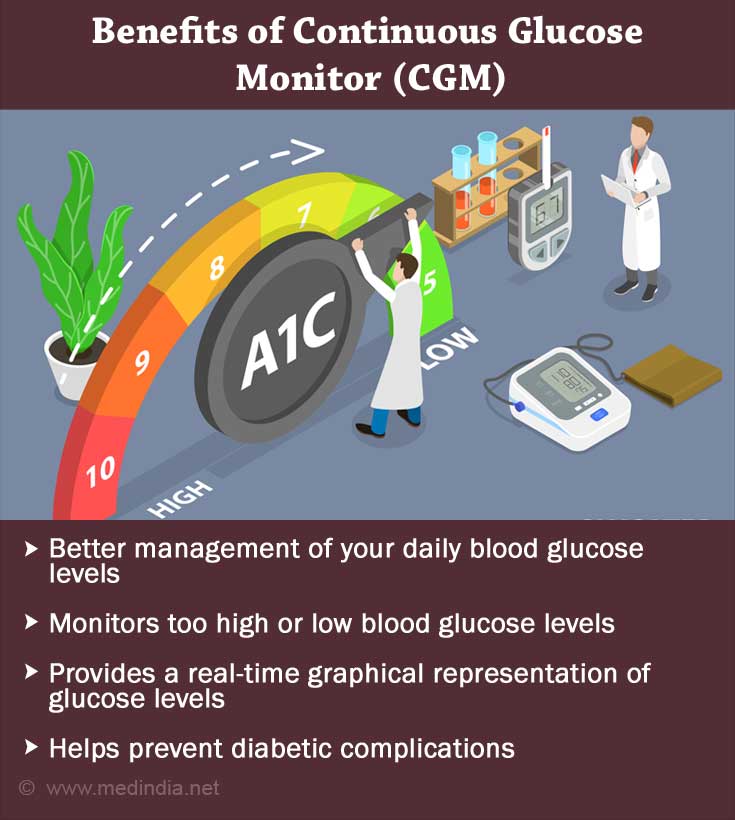
- Aids in better managing your daily blood glucose levels as they help track spikes between meals, early morning, and sleep.
- Useful for patients who are on intensive insulin therapy or often suffer from high or low blood glucose levels.
- With seamless monitoring of glucose levels, chances of low or high blood glucose emergencies are curbed drastically. CGMs help identify four times as many serious glucose incidents as a standard glucose meter.
- Provides a real-time graphical representation of targeting your ideal glucose levels.
- Helps prevent diabetic complications and promotes living for all diabetics patients.
What are the Limitations of Continuous Glucose Monitor?
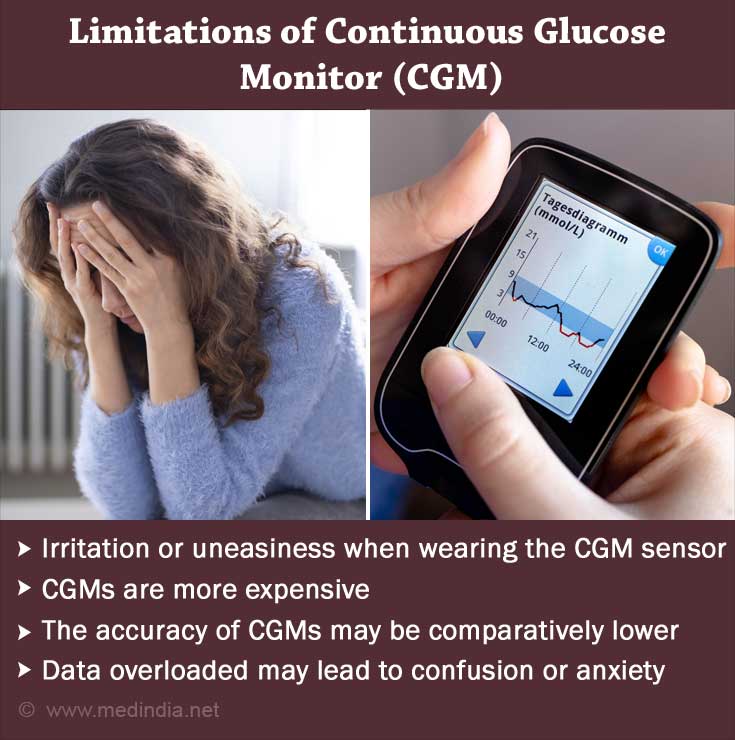
- Irritation or uneasiness when wearing the CGM sensor initially
- CGMs are more expensive when compared to a standard glucose meter
- Accuracy of some of the older models of CGM may interact when you are critically ill, on dialysis, pregnant, or taking certain medications like acetaminophen, lisinopril, and albuterol; hence, it is important to consult your physician before confirming your CGM results.
- Further accuracy is needed to limit the use of finger-stick glucose tests for standardizing and confirming the CGM results twice a day.
- Data overloaded may sometimes lead to confusion or anxiety.
- Improbability regarding different insurance coverage for the CGMs’ cost.