- KD Tripathi. Essentials of Medical Pharmacology
- Rabinowich L, Shibolet O. Drug Induced Steatohepatitis: An Uncommon Culprit of a Common Disease. BioMed Research International Volume 2015 (2015), Article ID 168905; http://dx.doi.org/10.1155/2015/168905
- Prasad R, Gupta P, Singh A, Goel N. Drug induced pulmonary parenchymal disease. Drug Discoveries & Therapeutics. 2014; 8(6):232-237
- Matsuno O. Drug-induced interstitial lung disease: mechanisms and best diagnostic approaches. Respiratory Research201213:39; https://doi.org/10.1186/1465-9921-13-39
Introduction
The term ‘drug-induced diseases’ sounds like a paradox. Drugs or medications are taken to treat diseases. The last thing one would expect is that the medication used to relieve discomfort would actually do harm! ‘Drug-induced diseases’ refer to those adverse effects of drugs that are serious enough for the patient to consult a doctor or get hospitalized. The effects may persist even after the treatment with the drug has been discontinued.
Adverse drug reactions are a reality. Then why do we use drugs? Drugs are approved for use only if their potential benefits far outweigh the risks involved. Also, not all people react similarly to a drug. It is possible that a particular drug, while completely benefiting some people may cause a potentially life-threatening adverse effect on some others!
Every drug undergoes extensive testing before it is introduced into the market. This includes testing in animals, and only once the safety and efficacy of the drug are established, it is tested in humans. Once approved, it is introduced into the market. Unfortunately, several adverse effects appear when the drug is introduced into the larger population. Many drugs have had label changes, introduction of black box warnings on their labels, or had to be withdrawn due to this reason. These adverse effects come to the notice of authorities either through spontaneous reporting by physicians, or various studies conducted.
What are the Types of Drug-Induced Diseases?
Diseases caused by drugs can be either predictable or unpredictable. Predictable effects are an extension of the normal pharmacological effects of the drug. For example, blood thinners (anticoagulant and antiplatelet drugs) that are used to prevent clotting of blood can cause bleeding as a side effect. Several anti-diabetes medications like insulin and sulfonylureas can cause low blood glucose levels.
On the other hand, unpredictable effects are completely unrelated to the therapeutic effect of the drug. For example, amiodarone, a drug used to treat abnormal heart rhythms, can cause lung damage.
Depending on their severity, drug-induced diseases may be classified as mild, moderate, severe, or lethal if they cause death.
Drug-induced diseases can affect various organ systems of the body. Several drugs have been banned because of their ability to cause serious diseases. The list of drugs that cause diseases can go on for several pages; here are some examples listed below according to the organ system affected:
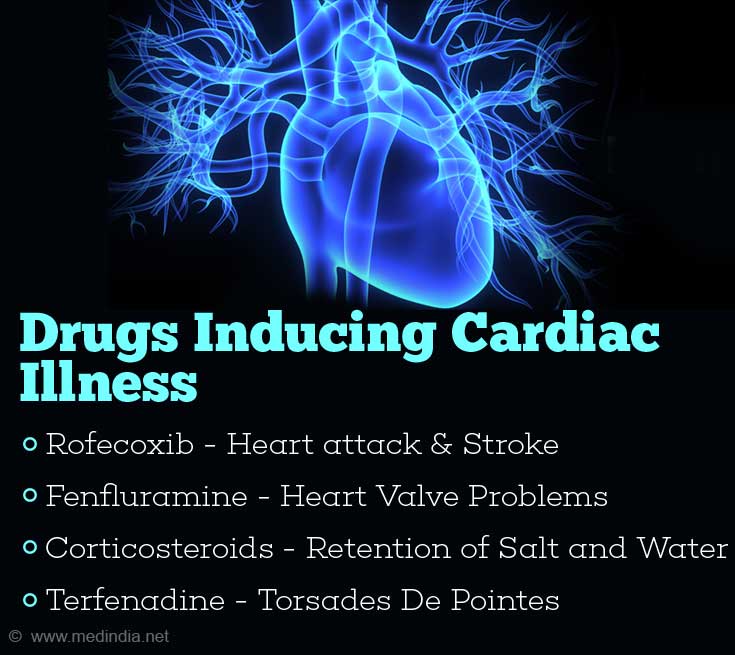
Cardiovascular system:
- Rofecoxib, a COX-2 inhibitor painkiller, was introduced with the hope that it would avoid the adverse effects of nonsteroidal anti-inflammatory drugs (NSAIDs) like stomach ulcers. Unfortunately, its use was associated with cardiovascular events like heart attack and stroke and the drug had to be withdrawn from the market.
- Several drugs used for the treatment of obesity met a similar fate. Fenfluramine and dexfenfluramine affected the heart valves, while sibutramine, was associated with cardiovascular events and stroke, and therefore had to be removed from the market.
- Several drugs have been associated with congestive heart failure. These include the anti-diabetes drug rosiglitazone, which should be avoided in patients who already suffer from heart failure. Drugs that slow down the heart like calcium channel blockers and beta blockers, and corticosteroids that cause retention of salt and water can also cause heart failure.
- Astemizole, terfenadine and cisapride can affect the electrical activity of the heart causing prolongation of the QT interval and resulting in a condition called torsades de pointes. The chances of this side effect are particularly high when one of these drugs is administered with drugs that prevent its breakdown like erythromycin and ketoconazole.
Skin:
The skin is the most obvious part of the body, and therefore any reaction is very easy to notice. Drug-induced skin reactions may be acute or chronic.
- The acute reactions may vary from a simple rash and itching to a serious condition like angioedema and Stevens-Johnson’s syndrome / toxic epidermal necrolysis. Drugs that often cause acute skin reactions include penicillin, sulfonamides, allopurinol (anti-gout medication) and those that treat seizures and mental illnesses like anticonvulsants and antipsychotics.
- A special type of skin reaction caused by drugs is called fixed drug eruption. Here, the skin lesion appears only on a particular part. Fixed-drug reactions are noted with tetracycline, barbiturates and sulfonamides.
- The blood-thinner warfarin can rarely cause necrosis of the skin.
- Sulfonamides, chloroquine and tetracycline can produce a photosensitivity reaction, which is a skin reaction that develops when the patient taking these drugs is exposed to sunlight. Therefore, patients on these medications are asked to avoid sunlight while being treated.
- Hydralazine and procainamide cause a chronic immunological reaction called SLE-like syndrome that also affects the musculoskeletal system, kidneys and the brain.
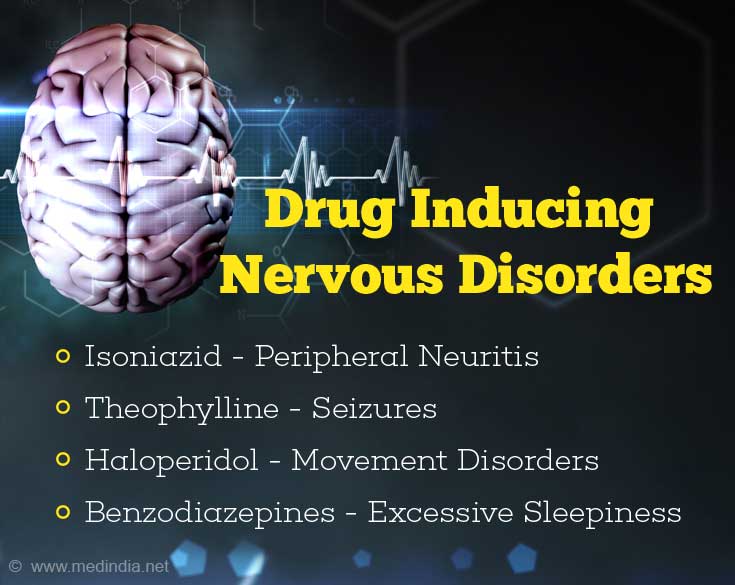
Brain and Nerves:
- The anti-tuberculosis drug isoniazid or INH interferes with the utilization of vitamin B6 and causes neurological symptoms ranging from peripheral neuritis, mental disturbances and rarely seizures.
- Theophylline, an anti-asthma medication, if not maintained within normal levels in the blood, can cause neurological symptoms like restlessness and tremors, which may also progress to seizures along with abnormal heart rhythms and shock.
- Some of the older antipsychotic drugs like fluphenazine and haloperidol can cause movement disorders like acute dystonia (abnormal muscle spasms) in the facial muscles, akathisia (a compulsion to move), Parkinsonism, malignant neuroleptic syndrome (which results in stiffness and tremor), and tardive dyskinesia which occurs later during therapy.
- Pregabalin, barbiturates and benzodiazepines can cause excessive sleepiness. Patients taking such drugs should avoid driving or using dangerous machinery while on the medication to prevent accidents.
Lung:
- Drugs used for the treatment of cancer, methotrexate and bleomycin cause scarring of the lungs called pulmonary fibrosis or interstitial pneumonitis. The patient suffers from breathlessness and non-productive cough, which can worsen if the dosage is not lowered. Amiodarone is a non-anticancer drug that also damages the lung.
- Aspirin and nonselective beta blockers like propranolol can cause an asthma-like condition, making it difficult for the patient to breathe. These should be avoided in patients with pre-existing asthma. In addition, any drug can cause a severe allergic reaction that mimics an asthmatic attack.
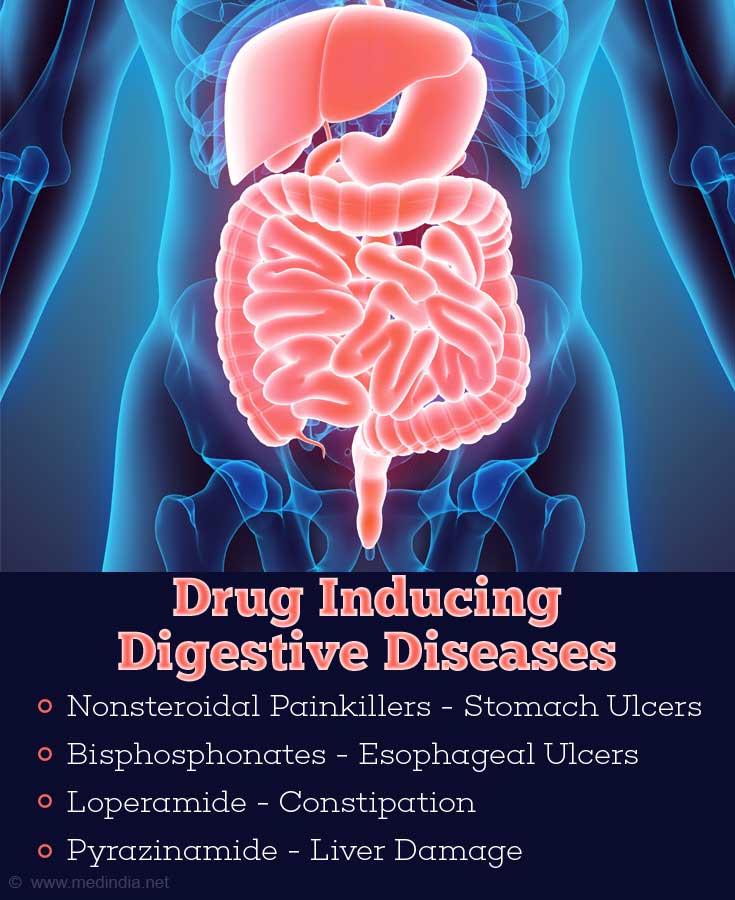
Digestive tract:
- Nonsteroidal painkillers and corticosteroids are well known to cause stomach ulcers, especially when taken on an empty stomach. Bisphosphonates used in the treatment of osteoporosis can cause esophageal ulcers and are advised to be taken in an upright position.
- Diarrhea can be caused by nearly every oral drug. Iron salts and loperamide can cause constipation.
- The liver is the site for detoxification. Some drugs, however, affect the liver causing serious problems. High dose of acetaminophen, an otherwise safe drug in normal doses, causes liver toxicity (hepatotoxicity). Several first-line anti-tuberculosis drugs that include INH, rifampicin and pyrazinamide cause liver damage, and reduce the options for the treatment of tuberculosis in these patients. Amiodarone, methotrexate, and valproic acid are some of the other hepatotoxic drugs. These drugs should be avoided in alcoholics and other patients who already suffer from liver disease. Troglitazone, an anti-diabetes medication was withdrawn due to its liver-damaging effect.
Genital and Urinary tract:
- Drugs can affect different parts of the kidney causing a number of kidney disorders. These include glomerulonephritis which may be caused by drugs like penicillin, NSAIDs, gold, lithium and hydralazine, acute tubular necrosis caused by drugs like aminoglycosides and amphotericin B, and acute interstitial nephritis caused by penicillin, NSAIDs and rifampicin. Cyclosporine and tacrolimus can cause chronic kidney failure. Damage to the kidneys may reduce the excretion of several drugs through the urine; hence these drugs may need to be avoided or may require dosage adjustment.
- Erectile dysfunction is a side effect of drugs like thiazide diuretics and antidepressants.
Blood:
- Drugs can produce anemia by reducing the production of red blood cells by the bone marrow (e.g. chloramphenicol, sulfonamides and carbamazepine), or destroying the formed red blood cells by a process called hemolysis (e.g. primaquine, penicillin and sulfonamides). Hemolysis is particularly a problem in patients with the deficiency of an enzyme called glucose-6-phosphatase.
- Some drugs reduce white blood cell counts and increase the chances of suffering from infections. These include methimazole, phenylbutazone and clozapine.
- Heparin has been associated with thrombocytopenia, a condition that lowers the platelet counts in the blood and increases the chances of bleeding.
Bone:
- Long-term use of glucocorticoids can weaken bones causing osteoporosis and increasing the risk of fractures.
- The anti-tubercular drugs ethambutol and pyrazinamide can increase the blood uric acid, causing a gout-like disease.
Hormonal conditions:
- Glucocorticoids raise blood glucose levels and cause a diabetes-like condition. Therefore, a history of drug intake is important in any individual who tests positive for high blood glucose.
- Amiodarone and lithium can cause thyroid problems.
Cancer:
- Hormone replacement therapies can cause breast cancer.
- Diethylstilbestrol caused vaginal adenocarcinoma in daughters of women who took the drug during pregnancy.
How are Drug-Induced Diseases Diagnosed?
Drug-induced diseases are primarily diagnosed based on the history of drug intake obtained from the patient or the family. The symptoms should appear at a reasonable time frame after taking the medication. By default, physicians should enquire about drug intake to any patient coming to the clinic with a problem so as not to miss out on a drug-induced disease. If the drug is re-administered the symptoms may reappear. This is referred to as re-challenge. Re-challenge confirms a drug-induced disease, but is usually not done due to ethical reasons.
How are Drug-Induced Diseases Treated?
The first step in the treatment of drug-induced diseases is to report the adverse effect to the physician who may stop the intake of the medication or at times, reduce the dose gradually, and replace with an appropriate alternative. Many times, this simple step can relieve the patient of the symptoms. Those who do not recover require additional treatments depending on the adverse event.
How do you Prevent Drug-Induced Diseases?
Steps that could help to prevent a drug-induced disease include the following:
- Always inform your doctor if you suffer from any illness or take any other medication including a nutritional supplement before you are prescribed a medication.
- Inform your doctor if you have suffered from any previous allergic reaction to a drug or any other substances like food ingredients.
- Take the medication only as prescribed by the doctor. Stick to the dose, duration of treatment as well as other instructions like taking it after meals.