- Lee WM. Drug-induced hepatotoxicity. N Engl J Med. 2003;349:474-485.
- Sturgill MG, Lambert GH. Xenobiotic-induced hepatotoxicity: mechanisms of liver injury and methods of monitoring hepatic function. Clin Chem. 1997;43(8):1512-1526.
- Hunt BJ. Bleeding and coagulopathies in critical care. N Engl J Med. 2014;370:847-859.
What is Hepatotoxicity?
Hepatotoxicity means damage to the liver caused by drugs and other factors resulting in problems in its functioning. Chemicals or drugs that cause hepatotoxicity are called hepatotoxins.
In the ancient world, the liver was considered as the organ that controlled our emotions and was the very crux of life. The Egyptians, Greeks, Shakespeare, have all sung the glories of the liver. A Nobel laureate from Chile, Pablo Neruda, even wrote a poem on the liver. So, you can imagine the importance of the liver in literature and this is hardly surprising. The liver is an organ that maintains the balance in our body. It is an organ where toxic compounds are detoxified, vitamins are stored, proteins, carbohydrates, and fats are broken down and bile acids are produced. The liver is also involved in molecular pathways involved in fighting infections, in reproduction, blood clotting and other functions. Any damage to the liver therefore can affect almost the entire body.
Drug-induced liver injury accounts for 5% of hospital admissions with jaundice and is the cause for nearly half of the acute liver failure cases. Women are normally more commonly affected by drug-induced liver injury compared with men.
Why is the Liver susceptible to Injury by Chemicals?
The liver is the major organ in charge of breaking down fats, proteins, carbohydrates, drugs, and practically anything that enters our body. Since the metabolism of drugs occurs in the liver, the toxic effects of the drug affect the liver. Chemicals (e.g. drugs, smoking, alcohol) and toxins (plant, viral, or bacterial) induce changes to the biochemical pathways in the liver cells, or induce an immune response, or make the liver cells extremely sensitive to the defence missiles or cytokines in the body. The cells of the bile duct are are also affected by exposure to hepatotoxic drugs. Some patients progress to cirrhosis and liver failure, or can even develop benign or malignant cancers. The type of liver injury caused by chemicals can vary from:
- Hepatocellular injury, where the cells of the liver are damaged.
- Cholestatic injury which occurs due to obstruction to the flow of bile through the bile ducts. As a result, bile acids accumulate in the liver, which can damage it
- Mixed, which has features of both hepatocellular and cholestatic injury
- Other forms of liver injury like immunological injury, which occurs due to an immune reaction and mitochondrial injury, which can result in serious liver failure
Factors that could increase the chance of hepatotoxicity by medications include:
- Presence of pre-existing liver disease like HIV, hepatitis B or hepatitis C, or due to alcohol intake
- Presence of diseases affecting other organs like kidney failure
- Intake of other liver-damaging medications or herbal products
- Age, gender, genetic factors and ethnicity of the individual. Women appear to be affected more commonly
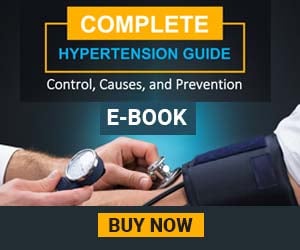
What are the Causes of Hepatotoxicity?
Several drugs can be hepatotoxic depending on their dosage and the patient characteristics. The hepatotoxic drugs include:
- Non-steroidal anti-inflammatory drugs like acetaminophen and nimesulide
- Anti-retroviral drugs like zidovudine, didanosine and stavudine used in the treatment of HIV
- Antituberculosis drugs like rifampicin, isoniazid and pyrazinamide
- Antibiotics like erythromycin
- Cholesterol-lowering drugs like pravastatin, lovastatin and niacin
- Anesthetic agents like halothane
- Anti-epileptic drugs like carbamazepine, valproic acid, felbamate and phenytoin
- Anti-rheumatic drugs like methotrexate and azathioprine
- Cocaine
- Antipsychotics drugs like chlorpromazine and haloperidol
- Antidepressant drugs like amineptine and imipramine
- Anti-Alzheimer’s drugs like tacrine
- Antihypertensive drugs like Methyldopa
- Oral contraceptives
Hepatotoxicity may also be caused by environmental chemicals like arsenic, or intake of alcohol.
What are the Symptoms and Signs of Hepatotoxicity?
There are 2 main types of hepatotoxicity – predictable (intrinsic) and idiosyncratic. Predictable injuries to the liver are dependent on the dose of the drug; they cause hepatotoxicity mainly at a higher dose. Idiosyncratic reactions are rare (1 in 1000 or 1 in 100 000 patients) and unpredictable drug reactions that occur at normal doses and often have serious consequences.
Symptoms of drug hepatotoxicity usually subside once the drug is withdrawn. They also depend on the type of liver injury and the degree of damage to the liver.
Symptoms of hepatotoxicity may include the following:
- Extreme exhaustion and fatigue
- Fever
- Jaundice: This is a classic symptom which causes the whites of the eyes, the skin, and the mucous membranes to become yellow.
- Severe itching
- Unusual increase in weight of over 1.5 to 2.5 kg in 1 week
- Swelling of feet and legs
- Nausea, vomiting, and pain in the abdomen
- Incessant bleeding in serious cases

How to Diagnose Hepatotoxicity?
Hepatotoxicity may be diagnosed in the following ways:
Biopsy of the liver: A small tissue of the liver is removed and observed under the microscope to determine the type and extent of damage to the cells of the liver.
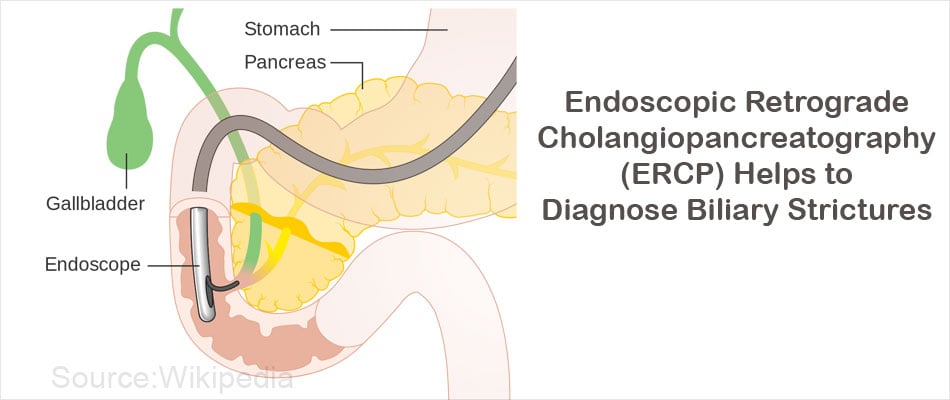
Endoscopic retrograde cholangiopancreatography (ERCP): This procedure is utilized to observe if the bile duct is blocked and is contributing to liver damage. As the name implies, an endoscope (a flexible tube with a light) is used to inject a dye into the biliary ducts. Any blockage in the bile duct is observed with the help of an x-ray.
Blood tests:
- Serum ALT (alanine aminotransferase) activity: This is a very sensitive test and biomarker for hepatotoxicity. It is termed “the gold standard clinical chemistry marker of liver injury”. The ALT enzyme is mainly found in the liver while minor quantities are observed in the skeletal muscle and heart. When the liver cells or hepatocytes are damaged, their contents are released into the bloodstream. Hence the levels of the ALT enzyme increase in the blood. Sometimes, injury to the skeletal muscle or heart can also drive up the levels of the ALT enzyme in the blood. Hence, there are chances of false positive results for hepatotoxicity in this test.
- Serum AST (aspartate aminotransferase) activity: The AST enzyme is present in the liver, heart, skeletal muscle, and brain. Like the ALT enzyme, the serum AST levels increase when hepatocytes are injured. Increased levels of the AST enzyme are also achieved when there is injury to organs other than the liver that contain the enzyme. This marker is not as specific as ALT. To confirm liver damage, the ratio of AST to ALT is measured.
There are other blood tests that are performed to supplement the results of the serum ALT test. They are listed below:
- Alkaline phosphatase activity: Any obstruction in the bile duct will lead to increased levels of alkaline phosphatase. Increased levels of ALP are a good indicator of drug-associated cholestasis in humans.
- Gamma-glutamyl transferase (GGT) levels: GGT levels in the blood also increase in cholestatic liver disease.
- Bilirubin and Bile acids: In the case of acute liver injury, bilirubin and bile acid levels may be increased in the blood.
- Other blood tests that are used to diagnose liver disease include measurement of serum albumin levels, serum 5¢ nucleotidase levels and prothrombin values.
Computed tomography scans (CT): In this test, the liver is scanned following injection of a radioactive dye into a vein. The three dimensional images obtained help to detect changes in the liver.
The history is an important diagnostic aspect of the diagnosis. The hepatotoxicity can more or less be assumed to be due to a drug if it occurred after intake of the medication, and if it improved after stopping the medication. It can be confirmed if the symptoms re-appear after re-instating the drug, but this is not done in clinical practice due to ethical reasons.
How do you Treat Hepatotoxicity?
The best way to avoid irreparable damage to the liver by a drug is to detect the toxic effects of the drug at its earliest stage, monitor and assess the damage, and decide on the line of treatment. Prompt attention will prevent the liver from being completely damaged to the point of no return.
The first step in treating hepatotoxicity caused by drugs is to stop taking the drug in question after consulting your doctor. Your doctor may prescribe medications to control certain symptoms. For example, the accumulation of fluid within the body can be reduced with diuretics. Cholestyramine may be used to treat itching.
N-acetylcysteine is prescribed for acetaminophen poisoning.
Liver transplantation may be required for severe liver injury.