- Sex Reassignment Surgery in the Female-to-Male Transsexual - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3312187/)
- Gender Affirmation Surgeries - (https://www.hopkinsmedicine.org/health/wellness-and-prevention/gender-affirmation-surgeries)
- Gender Confirmation Surgery - (https://www.uofmhealth.org/conditions-treatments/transgender-services/gender-confirmation-surgery)
- Klinefelter syndrome - (https://www.nhs.uk/conditions/klinefelters-syndrome/)
About
Gender reassignment surgery, also known as gender-affirming surgery, is a medical procedure or series of procedures aimed at altering an individual's physical appearance and sexual characteristics to align with their gender identity.
In Simple words, it can be defined as the alteration of a person's physical sex characteristics by surgery in order to match the person’s gender identity
This transformative process is often pursued by transgender individuals, as well as some cisgender and non-binary individuals. It involves various surgical interventions to modify primary and secondary sexual characteristics, thereby affirming an individual's gender identity(1✔ ✔Trusted Source
Sex Reassignment Surgery in the Female-to-Male Transsexual
Go to source).
Alternative Names for Gender-Affirming Surgery
- Gender reassignment surgery (GRS)
- Gender-affirmation surgery
- Gender confirmation surgery
- Sex reassignment surgery
Who Can Get Gender Reassignment Surgery?
Indications
- Transgender Individuals
- Intersex Individuals
- Drag Performers
- Individuals with Klinefelter Syndrome
- Non-Binary Individuals
- Cisgender
Is Gender Dysphoria the only Reason for Gender Reassignment Surgery?
No, not only gender dysphoric individuals seek gender reassignment surgery. While gender dysphoria is a common reason why individuals pursue gender-affirming surgeries, it's not the only factor. Some people may choose to undergo these surgeries for reasons beyond alleviating distress associated with gender dysphoria.
For example, individuals with intersex variations may seek gender-affirming surgeries to align their physical appearance with their gender identity, even if they do not experience gender dysphoria. Similarly, some non-binary individuals may opt for surgeries to achieve a physical presentation that better aligns with their gender identity, regardless of whether they experience gender dysphoria.
Furthermore, some cisgender individuals may also undergo gender-affirming surgeries for reasons related to body dysmorphia or dissatisfaction with their physical appearance, rather than gender dysphoria.
Ultimately, the decision to pursue gender reassignment surgery is deeply personal and can be influenced by a variety of factors beyond gender dysphoria alone.
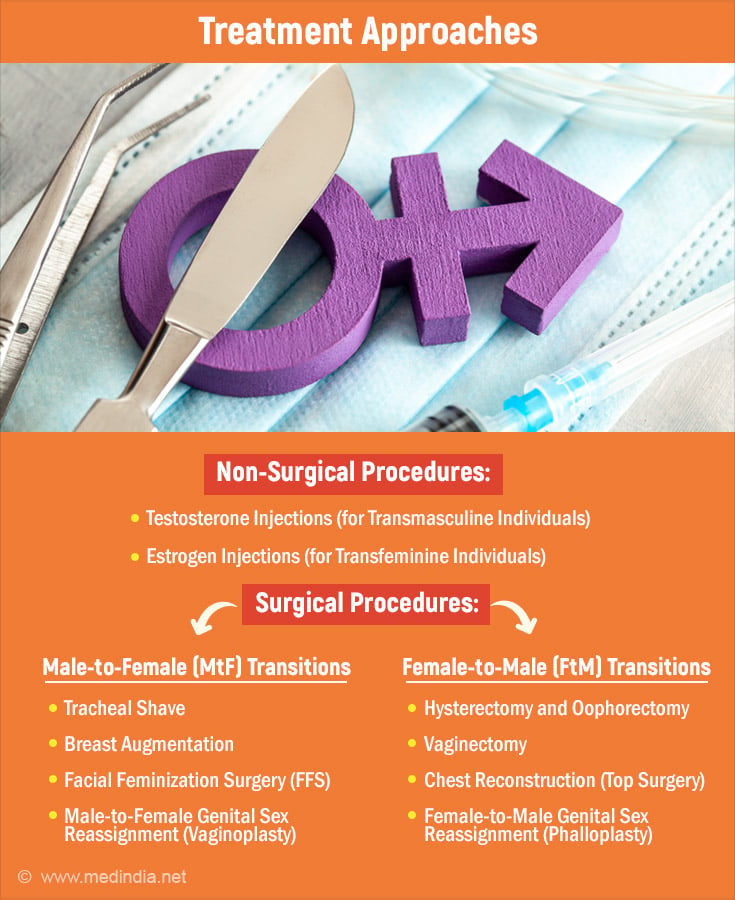
Non-Surgical Procedures
Hormonal injections is the only available non-surgical procedure.It isa form of hormone replacement therapy (HRT) commonly used in transgender healthcare to induce and maintain desired physical changes consistent with an individual's gender identity.
These injections typically involve the administration of testosterone for transmasculine individuals (female-to-male, or FtM) and estrogen for transfeminine individuals (male-to-female, or MtF).
Testosterone Injections (for Transmasculine Individuals)
Purpose: Testosterone injections are administered to induce masculine changes, such as increased facial and body hair growth, deepening of the voice, muscle development, and redistribution of body fat.
Types of Testosterone: There are different formulations of testosterone available for injection, including testosterone cypionate, testosterone enanthate, and testosterone undecanoate.
Administration: Testosterone injections are typically administered intramuscularly (into the muscle) in either the gluteal (buttocks) or deltoid (upper arm) muscle.
Dosage and Frequency: The dosage and frequency of testosterone injections can vary depending on individual factors such as age, weight, hormone levels, and desired changes. Typically, injections are administered every one to two weeks to maintain stable testosterone levels in the body.
Monitoring: Regular monitoring of hormone levels, liver function, and other relevant markers is essential to ensure the safety and effectiveness of testosterone therapy. Blood tests may be conducted periodically to assess hormone levels and adjust the dosage as needed.
Estrogen Injections (for Transfeminine Individuals)
Purpose: Estrogen injections are administered to induce feminine changes, such as breastdevelopment, redistribution of body fat, softening of the skin, and reduction of muscle mass.
Types of Estrogen: The most common form of estrogen used in injections is estradiol valerate.
Administration: Estrogen injections are typically administered intramuscularly, similar to testosterone injections, in the gluteal or deltoid muscle.
Dosage and Frequency: The dosage and frequency of estrogen injections vary depending on individual factors and treatment goals. Typically, injections are administered every one to two weeks.
Monitoring: Regular monitoring of hormone levels, liver function, and other relevant parameters is crucial for ensuring the safety and effectiveness of estrogen therapy. Blood tests may be conducted periodically to assess hormone levels and adjust the dosage as needed.
Time Frame of Use of Hormonal Injections
Initiation: Hormonal injections are often initiated after a thorough evaluation by healthcare providers, including discussions about treatment goals, potential risks and benefits, and informed consent. The timing of initiation may vary depending on individual factors such as age, readiness for treatment, and presence of any underlying health conditions.
Duration: Hormonal injections are typically used as part of long-term hormone replacement therapy to maintain desired physical changes and support overall well-being. The duration of hormone therapy may vary from individual to individual and often continues indefinitely, especially for those who desire ongoing maintenance of gender-affirming changes.
Discontinuation: In some cases, individuals may choose to discontinue hormonal injections for various reasons, such as personal preference, changes in health status, or the achievement of desired physical changes. It's essential for individuals to discuss any plans to discontinue hormone therapy with their healthcare provider to ensure proper management of any potential effects or complications.
Surgical Procedures: Gender Affirming Surgery
These surgical procedures play vital roles in gender affirmation for transgender individuals, aligning their physical appearance with their gender identity(3✔ ✔Trusted Source
Gender Confirmation Surgery
Go to source).
Male-to-Female (MtF) Transitions:
- Tracheal Shave: This procedure reduces the prominence of the Adam's apple, a typically male characteristic, to create a smoother, more feminine neck contour.
- Breast Augmentation: Transfeminine individuals undergo breast augmentation to develop fuller, more feminine breast contours. Breast implants are placed behind breast tissue or chest muscle to achieve the desired size and shape.
- Facial Feminization Surgery (FFS): FFS encompasses various surgical procedures aimed at feminizing facial features. Techniques may include forehead contouring, rhinoplasty, cheek augmentation, chin and jaw reshaping, tracheal shave, lip augmentation, and hairline lowering to achieve a more traditionally feminine appearance.
- Male-to-Female Genital Sex Reassignment (Vaginoplasty): This surgical procedure constructs female genitalia for transfeminine individuals seeking alignment with their gender identity. Techniques involve using penile and scrotal tissue to create the vaginal canal, labia, and clitoral hood. The procedure may also include the creation of a neurovascular neoclitoris, providing both aesthetic and functional female genitalia in one operation.
Female-to-Male (FtM) Transitions:
- Hysterectomy and Oophorectomy: This procedure involves the removal of the uterus and ovaries, reducing the production of female hormones (estrogen and progesterone).
- Vaginectomy: Vaginectomy is the surgical removal of the vaginal canal, aligning the physical anatomy with a masculine appearance.
- Chest Reconstruction (Top Surgery): FtM individuals undergo chest reconstruction surgery to remove breast tissue and reshape the chest to achieve a more masculine contour. Techniques include subcutaneous mastectomy or double mastectomy with or without nipple reconstruction.
- Female-to-Male Genital Sex Reassignment (Phalloplasty): Phalloplasty is a surgical procedure to construct a phallus for FtM individuals seeking male genitalia. The radial forearm flap method is commonly used, involving tissue grafting from the forearm to create the phallus and urethra for standing urination. This procedure can be performed concurrently with a hysterectomy/vaginectomy to complete the transition process. A scrotum with testicular implants may be constructed in a second stage.
These surgical interventions are integral to gender affirmation for transgender individuals, helping align their physical appearance with their gender identity and alleviating gender dysphoria. Each procedure is tailored to the individual's unique needs and goals, reflecting the diversity of experiences within the transgender community.
Risks in Non-Surgical and Surgical Procedures
Risks in Hormone Therapies
- Cardiovascular Risks: Hormone replacement therapy (HRT) may increase the risk of cardiovascular events such as heart attacks and strokes, especially in older individuals or those with pre-existing cardiovascular conditions.
- Thromboembolic Events: Estrogen therapy, particularly in forms like oral contraceptives, may elevate the risk of blood clots, leading to thromboembolic events such as deep vein thrombosis (DVT) or pulmonary embolism (PE).
- Endocrine Disruption: Hormone therapies can disrupt the body's natural hormone balance, leading to potential complications such as metabolic disturbances, including insulin resistance and dyslipidemia.
- Breast Cancer Risk: Some studies suggest that long-term use of hormone replacement therapy, especially estrogen-only formulations, may increase the risk of breast cancer in transgender women.
- Liver Dysfunction: Hormone therapies, particularly oral estrogen formulations, may affect liver function and increase the risk of liver disease or dysfunction.
Risks in Gender Reassignment Surgeries
- Surgical Complications: As with any surgical procedure, gender reassignment surgeries carry risks such as infection, bleeding, anesthesia complications, and adverse reactions to medications.
- Scarring: Gender-affirming surgeries, especially those involving breast augmentation, chest reconstruction, or genital reconstruction, may result in visible scarring that could impact body image and self-esteem.
- Loss of Sensation: Surgeries involving genital reconstruction, such as vaginoplasty or phalloplasty, may result in loss of sensation or altered sensation in the genital region, affecting sexual function and satisfaction.
- Functional Complications: Some individuals may experience functional complications post-surgery, such as urinary incontinence, erectile dysfunction, or difficulties with sexual arousal or orgasm.
- Psychological Impact: Gender reassignment surgeries can have profound psychological effects, including adjustment difficulties, post-operative depression, and challenges related to body image and identity.
Guidance on Surgical Procedures: Whom to Consult?
When contemplating gender reassignment surgery, it's essential for individuals to consult with a team of experienced healthcare providers specializing in transgender care. Here's whom to consider consulting:
1. Gender-Affirming Surgeons
Gender-affirming surgeons specialize in performing gender reassignment surgeries and have expertise in various surgical techniques, including chest surgery (for both masculinization and feminization procedures), genital reconstruction, and facial feminization surgery. These surgeons can provide comprehensive information about the surgical options available, discuss the potential risks and benefits, and guide individuals through the decision-making process.
2. Endocrinologists
Endocrinologists play a crucial role in managing hormone therapy for transgender individuals. They can provide guidance on hormone replacement therapy (HRT), including the use of testosterone for transmasculine individuals and estrogen for transfeminine individuals. Endocrinologists can assess hormone levels, monitor any potential side effects, and adjust hormone regimens as needed to support the transition process.
3. Mental Health Professionals
Mental health professionals, such as psychologists, psychiatrists, or licensed therapists, offer invaluable support throughout the gender transition journey. They can assist individuals in exploring their gender identity, coping with gender dysphoria, and addressing any psychological concerns or challenges that may arise before, during, or after surgery. Mental health professionals also play a role in assessing readiness for surgery and providing pre- and post-operative counseling and support.
4. Primary Care Physicians
Primary care physicians are essential members of the healthcare team and can provide general medical care, coordinate referrals to specialists, and monitor overall health and well-being. They can also assist with managing any pre-existing medical conditions and ensuring that individuals are physically fit for surgery.
5. Support Groups and Advocacy Organizations
Support groups and advocacy organizations within the transgender community can offer valuable peer support, resources, and information about gender-affirming surgeries. These groups provide opportunities for individuals to connect with others who have undergone similar experiences, share insights, and seek guidance from those who have navigated the transition process.
Consulting with a multidisciplinary team of healthcare providers ensures that individuals receive comprehensive care tailored to their unique needs and goals. This collaborative approach helps individuals make informed decisions about gender reassignment surgery and supports their overall health and well-being throughout the transition process.
Pre-operative Considerations
1. Medical Considerations
Transgender individuals may have preexisting health conditions like diabetes, asthma, or HIV, which can impact their eligibility for surgery and postoperative care. Surgeons often consult with endocrinologists to assess the patient's physical fitness for surgery, especially considering the complex medication regimens involved in hormone therapy before and after surgery.
2. Fertility Concerns
Patients considering sex reassignment surgery (SRS) are informed about potential infertility, particularly if procedures like orchiectomy or oophorectomy are performed as part of the transition process. Preservation of fertility options may be discussed before surgery.
3. Age and Consent
SRS is generally not performed on children under 18, with rare exceptions made for adolescents based on healthcare provider assessments and potential benefits or risks. Consent from parents or legal guardians is required, along with long-term mental health counseling to confirm persistent gender dysphoria.
4. Intersex and Trauma Cases
Infants born with intersex traits may undergo surgical interventions at or near birth, raising ethical concerns about human rights implications. Trauma cases also require careful consideration, as surgically assigned gender may not align with the individual's gender identity, leading to negative outcomes later in life.
5. Standards of Care
Many regions follow Standards of Care for the Health of Transgender and Gender Diverse People (SOC), such as those published by the World Professional Association for Transgender Health (WPATH). These guidelines outline minimum requirements for treatment, including psychological evaluation and living as the desired gender before surgery.
6. Insurance Coverage
Obtaining insurance coverage for SRS may require documented assessments by mental health professionals, evidence of persistent gender dysphoria, and completion of physician-supervised hormone therapy for a specified duration.
Post-operative Considerations
1. Quality of Life and Physical Health
Studies assessing postoperative quality of life vary, with some reporting similar quality to control groups while others note lower quality in domains of health and limitations. Overall, many individuals report improvements in mental health, satisfaction with physical appearance, and overall well-being after surgery.
2. Psychological and Social Consequences
SRS has been shown to be effective in relieving gender dysphoria, though some studies highlight methodological limitations. Patients often report reduced anxiety, depression, and hostility levels post-surgery, with improvements in self-perceived physical and mental health.
3. Sexuality and Sexual Satisfaction
SRS can significantly impact individuals' sexual experiences and satisfaction. Most transsexual individuals report enjoying better sex lives and improved sexual satisfaction after surgery, with changes in orgasm frequency, intensity, and masturbation habits observed. However, satisfaction levels may vary between trans men and trans women, and expectations for sexual aspects of life may differ from cisgender individuals.
4. Continued Support
Comprehensive postoperative care involves ongoing psychological support, management of any complications, and assistance with adjustment to physical changes. Social support networks play a crucial role in helping individuals navigate their post-surgical experiences and integrate their gender identities into their daily lives.
Impact on Mental Health
The denial or limited access to gender-affirming surgeries can have severe consequences for the mental health and well-being of transgender individuals.
1. Persistent Gender Dysphoria
Without access to surgery, transgender individuals may continue to experience intense distress and discomfort due to the misalignment between their gender identity and physical characteristics. This persistent gender dysphoria can lead to heightened anxiety, depression, and a sense of hopelessness.
2. Heightened Anxiety
Living in a body that does not align with one's gender identity can contribute to persistent anxiety. The frustration of being unable to access necessary medical care and the ongoing struggle to navigate societal expectations can exacerbate feelings of stress and worry.
3. Increased Depression
Untreated gender dysphoria and the inability to undergo gender-affirming surgeries can lead to deepening feelings of depression and despair. Transgender individuals may struggle with low self-esteem, feelings of worthlessness, and a sense of isolation from not being able to live authentically.
4. Social Withdrawal
The distress caused by the incongruence between one's gender identity and physical appearance can result in social withdrawal and avoidance of social interactions. Transgender individuals may feel ashamed or uncomfortable in social settings, leading to further isolation and loneliness.
5. Suicidal Ideation
The lack of access to gender-affirming surgeries and the ongoing struggle with gender dysphoria can significantly increase the risk of suicidal thoughts and behaviors. Without the hope of being able to live authentically and alleviate their distress, transgender individuals may experience profound feelings of hopelessness and desperation.
Click here to know more about Mental health in transgender community
Affordable Surgery Options
Gender-affirming surgeries, including gender reassignment surgery (GRS), vary widely in cost globally. Affordable options exist in countries like Turkey, Brazil, Argentina, and Belgium. Turkey offers the most budget-friendly option, followed by Brazil, Argentina, and Belgium. While these countries provide competitive prices, individuals should consider factors beyond cost, such as healthcare quality and legal protections.
In summary, gender reassignment surgery serves as a vital tool in validating the gender identities of transgender and intersex individuals, enabling them to harmonize their external appearance with their innate sense of self. Despite its transformative potential, many face obstacles in accessing this essential care, including financial constraints, inadequate insurance coverage, and legal hurdles.
As society progresses towards greater awareness and acceptance of transgender rights, it's imperative to prioritize equitable access to gender-affirming treatments and offer unwavering support to individuals throughout their transition journey. By dismantling these barriers and fostering inclusivity within healthcare systems, we can empower transgender individuals to live authentically and flourish in their gender identity.