- Endoscopic Ablation Shows Promise in Reducing Hunger and Promoting Weight Loss - (https://news.ddw.org/news/endoscopic-ablation-shows-promise-in-reducing-hunger-and-promoting-weight-loss/)
- Endoscopic Gastric Mucosal Ablation as a Primary Obesity Therapy (COMET) - (https://classic.clinicaltrials.gov/ct2/show/NCT05486338)
About
Endoscopic Mucosal Ablation (EMA) is a minimally invasive medical procedure used to treat conditions by selectively targeting and removing abnormal or diseased tissue from the mucosal lining of organs, typically performed using an endoscope.
In weight management, EMA specifically targets the gastric fundus, a region of the stomach responsible for producing ghrelin, the "hunger hormone." By ablating or destroying ghrelin-producing cells in this area, EMA aims to reduce ghrelin levels and suppress hunger, facilitating weight loss in individuals with obesity(1✔ ✔Trusted Source
Endoscopic Ablation Shows Promise in Reducing Hunger and Promoting Weight Loss
Go to source).
Ghrelin and its Role in Weight Regulation
Ghrelin,the "hunger hormone," plays a crucial role in regulating appetite and, consequently, body weight. Produced primarily in the stomach, ghrelin levels fluctuate throughout the day in response to feeding patterns and nutritional status.
When the stomach is empty, ghrelin levels rise, signaling hunger to the brain and stimulating appetite. Conversely, as the stomach fills with food, ghrelin secretion decreases, promoting feelings of satiety and reducing the urge to eat.
In individuals with obesity, ghrelin levels are often dysregulated, contributing to increased appetite and difficulty in controlling food intake. This dysregulation perpetuates a cycle of overeating and weight gain, making weight management challenging.
Understanding the intricate interplay between ghrelin and appetite regulation is essential for developing effective strategies for weight loss and obesity management. By targeting ghrelin production through interventions such as the endoscopic procedure described, it becomes possible to modulate hunger signals and facilitate sustainable weight loss(2✔ ✔Trusted Source
Endoscopic Gastric Mucosal Ablation as a Primary Obesity Therapy (COMET)
Go to source).
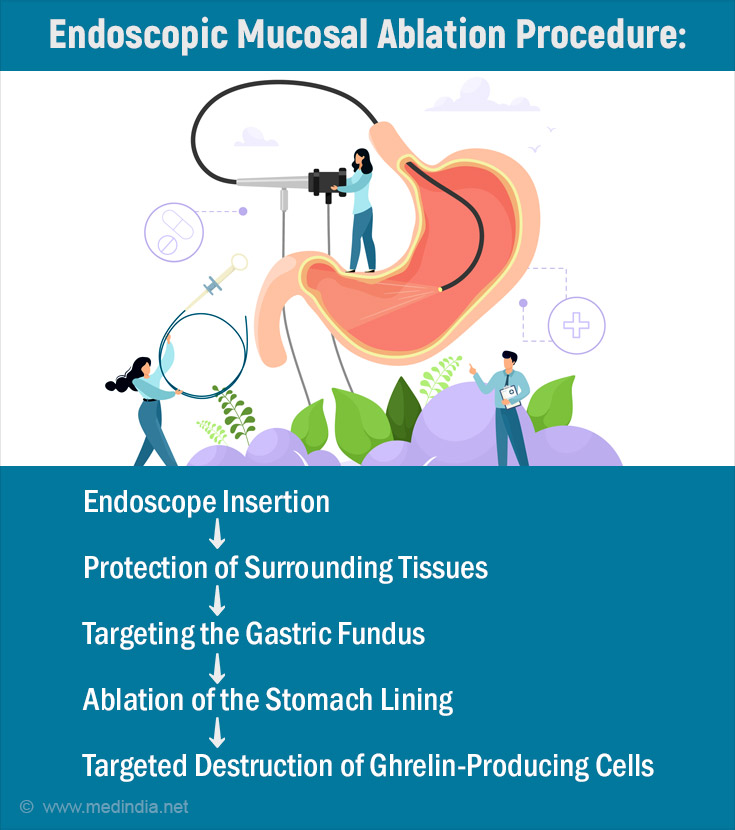
Endoscopic Mucosal Ablation Procedure
Endoscopic mucosal ablation procedure for burning the stomach lining to reduce the hunger hormone.
Step 1: Patient Preparation
Before the procedure begins, the patient is typically given instructions regarding fasting and medication usage. They may be required to refrain from eating or drinking for a certain period before the procedure. Additionally, the patient's medical history is reviewed, and any relevant allergies or pre-existing conditions are noted.
Step 2: Anesthesia Administration
To ensure patient comfort during the procedure, anesthesia is administered. This can vary from local anesthesia, which numbs the throat, to conscious sedation or general anesthesia, depending on the patient's needs and the complexity of the procedure.
Step 3: Endoscope Insertion
Once the patient is adequately sedated or anesthetized, an endoscope-a thin, flexible tube with a camera and light at the tip-is inserted into the mouth and guided down the esophagus into the stomach. The endoscope allows the gastroenterologist to visualize the internal structures of the stomach in real-time.
Step 4: Protection of Surrounding Tissues
To protect the surrounding tissues of the stomach from the thermal energy used during ablation, a protective fluid or solution is introduced into the stomach. This fluid helps prevent damage to healthy tissues adjacent to the targeted area.
Step 5: Targeting the Gastric Fundus
The gastroenterologist guides the endoscope to the upper portion of the stomach, specifically targeting the gastric fundus. This region is where ghrelin, the hunger hormone, is primarily produced. Precise navigation and positioning of the endoscope ensure accurate targeting of the desired area.
Step 6: Ablation of the Stomach Lining
Once the gastric fundus is identified, a specialized device attached to the endoscope is used to deliver thermal energy to the mucosal lining of the stomach. This energy source, often in the form of heat or radiofrequency waves, is carefully applied to selectively destroy or ablate the ghrelin-producing cells within the mucosa.
Step 7: Monitoring and Assessment
Throughout the procedure, the gastroenterologist monitors the ablation process via the endoscope's live video feed. Any adjustments to the energy delivery or positioning of the device can be made as necessary to ensure thorough treatment of the targeted area while minimizing damage to surrounding tissues.
Step 8: Post-Procedure Care
Once the ablation is completed, the endoscope is slowly withdrawn from the patient's body. Post-procedure care instructions are provided, including any dietary restrictions or activity limitations. Patients are typically observed in a recovery area until they are fully awake and stable before being discharged home.
Step 9: Follow-Up
Follow-up appointments are scheduled to monitor the patient's progress and assess the effectiveness of the procedure. This may include evaluating weight loss, changes in appetite, and any potential side effects or complications.
Indications
- Obesity: Endoscopic mucosal ablation may be indicated for individuals with obesity who have not achieved sufficient weight loss through conventional methods such as diet and exercise.
- Elevated Ghrelin Levels: Patients with elevated ghrelin levels, indicating dysregulation of hunger signaling, may benefit from this procedure.
- Desire for Minimally Invasive Treatment: Patients who prefer minimally invasive procedures over surgical interventions may opt for endoscopic mucosal ablation.
Comparative Analysis of EMA
Comparative analysis involves evaluating endoscopic mucosal ablation (EMA) against other weight loss interventions to determine the most appropriate option for individual patients.
- EMA vs. Bariatric Surgery: While bariatric surgery typically yields more significant and sustained weight loss, EMA offers a less invasive alternative with potentially lower risks and quicker recovery times. However, the efficacy of EMA may be less pronounced compared to surgery.
- EMA vs. Pharmacological Treatments: Compared to pharmacological treatments, which often target appetite suppression or fat absorption, EMA directly addresses the physiological mechanism of hunger by reducing ghrelin production. This targeted approach may offer unique benefits for certain patients.
- EMA vs. Lifestyle Interventions: EMA complements traditional lifestyle interventions such as diet and exercise by providing an additional tool for weight loss. However, its efficacy may vary depending on individual patient factors and adherence to post-procedure recommendations.
Relapse after Endoscopic Mucosal Ablation Procedure
Weight regain or relapse is a common challenge faced by individuals following any weight loss intervention, including endoscopic mucosal ablation (EMA). Several factors contribute to relapse, and proactive measures are needed to address this issue effectively.
- Physiological Factors: Changes in metabolism, hormone levels, and appetite regulation may contribute to weight regain over time, highlighting the importance of ongoing monitoring and management of these factors.
- Behavioral Factors:Adherence to dietary and lifestyle recommendations, as well as addressing emotional or psychological triggers for overeating, is critical for preventing relapse.
- Support Systems: Access to support groups, counseling services, and ongoing follow-up care can provide patients with the resources and encouragement needed to maintain their weight loss success.
- Reassessment and Adjustment: Regular reassessment of treatment goals and strategies, along with the flexibility to adapt the approach as needed, can help patients navigate challenges and sustain their progress over the long term.
Complications
- Bleeding: There is a risk of bleeding during or after the procedure, particularly if the mucosal lining is damaged excessively.
- Perforation: In rare cases, perforation of the stomach lining may occur, leading to leakage of gastric contents into the abdominal cavity.
- Infection: As with any invasive procedure, there is a risk of infection at the site of intervention.
- Pain and Discomfort: Patients may experience mild to moderate pain or discomfort following the procedure, which can typically be managed with pain medication.
Advantages
- Minimally Invasive
- Outpatient Procedure
- Targeted Approach
- Potential for Weight Loss
Disadvantages
- Limited Long-Term Data on the efficacy and safety of endoscopic mucosal ablation for weight loss.
- Potential for Ghrelin Rebound
- Additional research is needed to optimize patient selection criteria, refine procedural techniques, and assess long-term outcomes.
- The cost of endoscopic mucosal ablation may be a consideration for some patients, especially if it is not covered by insurance.
In summary, endoscopic mucosal ablation presents a beacon of hope in the realm of weight management, offering a tailored solution to the complex issue of obesity. Its ability to precisely target ghrelin production, coupled with its minimally invasive nature, underscores its potential as a transformative tool in combating obesity-related challenges.
As we continue to reveal the intricacies of this procedure and accumulate further evidence of its efficacy and safety, the promise it holds for individuals struggling with obesity grows ever brighter. Endoscopic mucosal ablation stands as a testament to the relentless pursuit of innovative solutions in the fight against obesity, offering renewed optimism for those seeking sustainable weight loss strategies.
With ongoing advancements and refinement, endoscopic mucosal ablation has the potential to redefine the landscape of weight management interventions, ushering in a new era of personalized care and improved outcomes for individuals worldwide. As we stand on the cusp of this transformative journey, the future looks promising, filled with renewed possibilities for healthier, happier lives.











