What is Corpectomy?
Corpectomy is a surgery to remove degenerative vertebrae along with the intervertebral discs that cause compression of the spinal cord and the nerves that arise from it.
General anatomy of the vertebral column:
The vertebral column in humans consists of 24 vertebrae that lie stacked one on top of the other. The 24 articulating vertebrae are divided into 3 regions comprising of the cervical (7 in number), thoracic (12 in number) and lumbar (5 in number) vertebrae. The vertebrae are separated by intervertebral disks, which act as shock absorbers.
The spinal cord extends from the base of the skull to the lower back through a canal formed by an opening in each stacked vertebra. The spinal cord transmits the information between the brain and the rest of the body through nerves that branch out through openings in the vertebrae.
There are eight pairs of cervical nerves, twelve pairs of thoracic nerves, and five pairs of lumbar nerves.
Depending on the location of the corpectomy, corpectomy can be classified as:
- Cervical corpectomy, in which the damaged vertebrae and intervertebral discs are surgically removed through the front of the neck
- Thoracic corpectomy, which is done in the chest region
- Lumbar corpectomy, which is done on the lower back
What are the Indications for Corpectomy?
Indications for corpectomy include the following:
- Spinal stenosis. Degenerative changes sometimes occur in the intervertebral discs of the spine and the joints around each vertebra. This may cause stenosis or narrowing of the spinal canal, the canal through which the spinal cord passes, and could result in pain.
- Damage to the vertebrae due to trauma, tumors, infections or deformity
A corpectomy is not always the first option for neck or back pain and is performed only when
- Non-operative measures such as pain medications and physical therapy are not effective
- The spinal cord is at risk of damage
- The pain is severe
- There is numbness / weakness in the legs and arms, loss of bladder control, and / or difficulty with walking and coordinated movements due to the spinal cord compression
How Should You Prepare for Corpectomy?
Your doctor will examine you and confirm the need for the surgery by conducting tests like a CT scan or an MRI.
For a CT scan, you will be asked to lie down still on a special table for a few minutes. A doughnut-shaped instrument will pass over the part to be screened, and images will be taken. A contrast may be injected into your vein; therefore you should inform the radiologist if you suffer from any allergies.
For an MRI, you will be placed inside a narrow tube, which can sometimes make you claustrophobic, if you have a fear of enclosed spaces. Few centers do offer more open MRI machines, but the drawback is that the pictures may not be as clear. The MRI machine makes loud clicking noises and it is advisable to ask for earplugs to help block these noises out.

- Your doctor has to be informed of all medications that you are taking (especially medications that can thin your blood such as aspirin) including over-the-counter medications and supplements. Your doctor may ask you to stop some of these a few days before the surgery.
- Allergies to any medications, foods or latex should be informed.
Routine tests:
All patients who undergo an elective surgery (which is more planned) require routine tests which include the following:
- Blood tests like hemoglobin levels, blood group, liver and kidney function tests
- Urine tests
- ECG to study the electrical activity of the heart
- Chest x-ray
In older group of patients, a detailed assessment of the heart maybe required.
Type of Anesthesia - Corpectomy is done under general anesthesia. You will be asleep during the procedure and will not be aware of what is going on.
Pre-operative Check-up – Routine tests as indicated above are ordered a few days before the surgery. Admission is required a day or two before the surgery.
Fasting before surgery - Overnight fasting is required and occasionally intravenous fluid maybe required to keep you well hydrated. Sedation is sometimes required for good overnight sleep before the surgery.
Shift from the ward or room to the waiting area in the operating room- An hour or two before the surgery, you will be shifted to the operating room waiting area on a trolley.
Once the surgical room is ready, you will be shifted to the operating room.
Shift to the Operating room- The ambiance in the operating room can sometimes be very daunting and a small amount of sedation can help overcome your anxiety. From the trolley, you will be shifted on to the operating table. As you look up, you will see the operating light console and at the head end will be the anesthesia machine. There may also be monitors to check oxygen levels, ECG and other vital parameters. A constant beeping sound may be present from the monitors, which may sometimes be irritating.
Anesthesia before surgery - The anesthetist will inject drugs through an intravenous line and make you inhale some gases through a mask that will put you in deep sleep for anesthesia. Once you are in deep sleep, a tube will be inserted into your mouth and windpipe to administer the anesthesia gases to overcome pain and keep you comfortable.
What Happens During a Corpectomy?
"Corpus" means body and "ectomy" means remove.
In corpectomy, the largest part of the damaged vertebra is removed including the vertebral bodies and the discs between the vertebrae, and the remaining vertebrae on both sides are fused together using a bone graft.
The procedure is performed in two steps:
1. Decompression
- The incision is made either on the anterior or posterior aspect depending on the planned approach.
- The muscles and other tissues are moved aside in order to reveal the bones of the spinal column. The arteries, nerves and other structures are protected from injury as well.
- An X-ray is used to identify the right disc(s) and right vertebra(e) to be removed.
- The surgeon then removes discs both above and below the damaged vertebra, followed the removal of the damaged vertebrae all the way back to the decompression, This procedure, called decompression, relieves the pressure on the spinal cord and nerves.
- Any bone spurs found sticking off the back of the vertebra are removed as well, taking great care all the time not to damage the spinal cord and nerve roots.
2. Spinal fusion
The space created due to the removed vertebrae has to be filled up with an implant that will provide strength and stability to the spine.
One type of implant is a structural bone graft or a strut graft. This is a piece of bone 1-2 inches in length taken from the pelvis or the leg bones of the patient (autograft) or from a bone bank (allograft). The strut graft is inserted into the available space in the spinal column and is fixed in place with titanium screws and plates. The bone graft will hold the remaining vertebrae apart and as it heals, it will eventually fuse, or grow together with the bone that is native to the area. Good bony fusion is important for long-term spinal stability.
Another type of implant is a cage or an artificial (manufactured) implant that can be inserted into the space and fixed in place with screws and plates. Cages are made completely of materials like titanium, ceramic, or man-made bone. Small bone grafts typically taken directly from the removed vertebra are used to help achieve fusion between the cage and the bone of the spinal column.
An internal fixation is sometimes necessary to hold the vertebra and the bone graft in place for which a metal plate is placed on the front of the spine and is attached to both the remaining vertebrae and the strut graft with metal screws.
The incision is then closed with sutures and dressed with a small gauze bandage. A drain will be left behind to drain off excess fluid.
Waking up from Anesthesia – Once the surgery is over, you will wake up and the tube down the wind pipe will be removed. You will be asked to open your eyes before the tube is removed. You will be sedated and the voice of the anesthetist may be faint. Once the tube is out, you may have cough and sometimes nausea.
There may be a tube going into the stomach called a nasogastric or Ryle’s tube to keep it empty. There will also be an intravenous line. You will remain on oxygen. Once fully awake, you will be shifted on the trolley and taken to the recovery room.
Recovery after Corpectomy
Recovery room – In the recovery room, a nurse will monitor your vitals and observe you for an hour or two before shifting you to the room or a ward.
Painkillers may be prescribed depending on the extent of the pain.
Post-operative recovery - You will remain in the hospital for a few days following the procedure. Intravenous lines for fluids and drugs will continue for a few days till you start eating normally.
You will probably be restricted to minimal activity during the early healing phases following the surgery.
A halo jacket will be used to hold your head perfectly still while the healing occurs and the vertebrae fuse. However, while you are in a halo jacket, you will not be able to do much rehabilitation.
You should work to keep your arm and leg strength intact.
A physical therapist will help you with an exercise routine.
DVT Prophylaxis – Early movement of your legs and some mobilization prevents DVT or deep vein thrombosis, where a clot is formed in the deep veins of the legs. The clot can travel up to the lungs and even be fatal. Other measures like small dose of heparin and special stockings may also be used to prevent DVT.
Chest physiotherapy maybe started after 24 hours to prevent chest infection.
Once the fusion is healed, you may progress on to a more vigorous rehabilitation program.
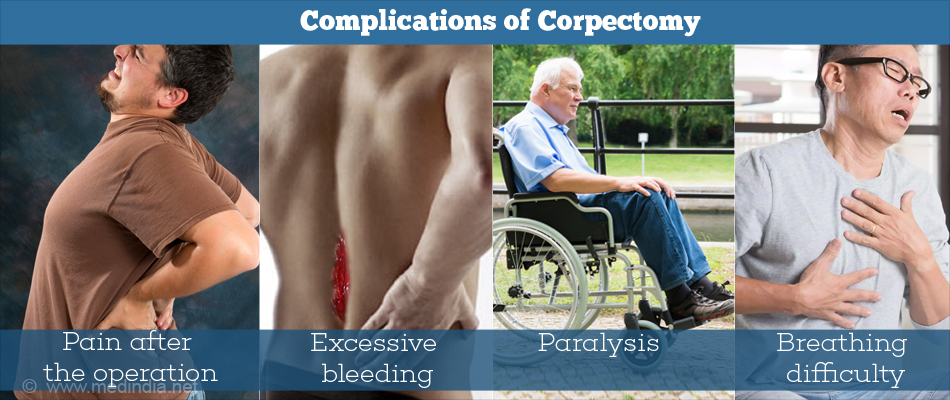
What are the Complications of Corpectomy?
Possible complications of corpectomy include the following:
- Failure to relive symptoms with persistence or increase of pain after the operation.
- Excessive bleeding.
- Infections occur in less than 1% of spinal surgeries and are of two kinds. Superficial or skin incisions are caused when the wound does not heal. It causes flu-like symptoms and can be treated with antibiotics. Deep wounds involving the spinal cord and vertebrae need additional operations to drain the infection and maybe remove the screws and plates.
- Hardware fracture can occur when the hardware used in the procedure break before the surgical site is completely healed.. Hardware fracture could result in broken or loosened plates and screws.
- Implant migration (graft displacement) can occur where the implant moves away from the attached position. If it moves too far, it may not be able to do its job of stabilizing the two vertebrae and, by moving in a direction towards the spine or large vessels, may damage these structures.
- Increased risk of damage to the spinal cord or nerve roots (nerve injury) which could result in paralysis.
- Degeneration of the intervertebral disks above or below the surgery level is known as transitional syndrome and is due to stress on the spinal segment adjacent to where the operation has taken place. Over time, this can lead to increased wear and tear to this segment, eventually causing pain
- Pseudoarthrosis, or motion between the two bones that should have been fused together, that results in continued pain.
- Difficulty in swallowing, soreness, voice changes and breathing difficulty in anterior cervical spine operations.
- Hip pain if the bone graft was obtained from the hip
- Nonunion of the spinal fusion