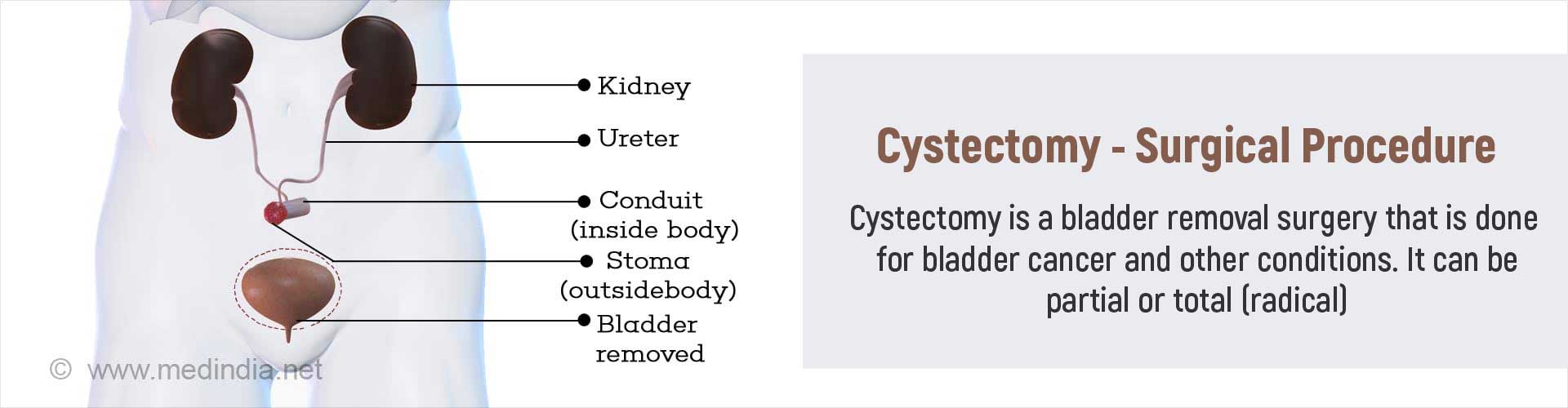
What is Cystectomy?
Cystectomy is a surgical procedure where the urinary bladder is removed, either partially (partial cystectomy) or completely (radical cystectomy) along with some surrounding structures. The procedure is performed as an open surgery or as a minimally invasive surgery through laparoscopy or robotic surgery. Following the removal of the bladder, a diversion for the urine from the body is also created during the same surgery.
Urinary Bladder - Anatomy
The urinary bladder is a triangular muscular bag located in the pelvic region. The urine produced by the kidneys reaches it via two narrow tubes called the ureters. The bladder stores the urine temporarily till it can be emptied through the urethral opening. Sphincters (circular muscle surrounding orifices) control the passage of urine through the urethra.
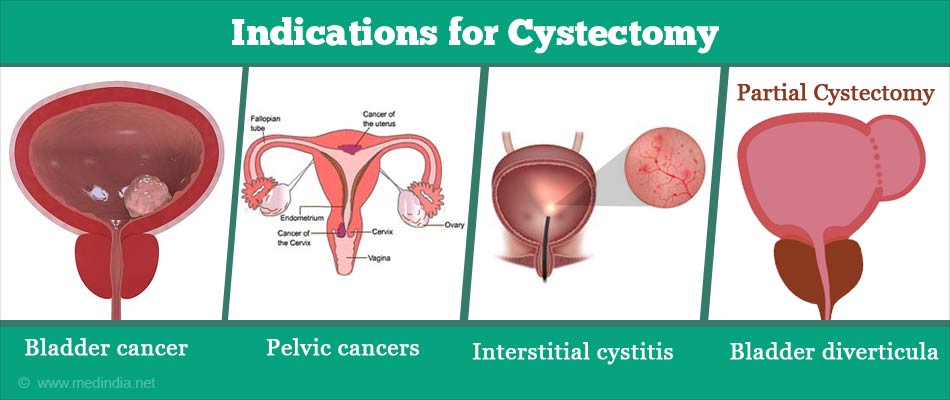
What are the Indications for Cystectomy?
Cystectomy is done for the following conditions:
Cancers, which include:
- Bladder cancer that invades the muscle but remains confined to the bladder
- Other pelvic cancers, such as advanced colon, prostate or endometrial cancer where the bladder is removed along with other organs
Non-cancerous conditions, which include:
- Severe interstitial cystitis that does not respond to other treatments.
- Developmental abnormalities of the bladder
- Bladder diverticula (outpouchings within the inner wall of the bladder).
- An abnormal connection (fistula) between the colon or the vagina and the bladder.
- Localized endometriosis of the bladder. Endometriosis of the bladder is when the tissue that normally lines the uterus occurs in other organs, in this case, in the bladder
- Other conditions like pheochromocytoma, schwannoma or endocervicosis involving the urinary bladder
- The presence of symptoms like severe blood loss in urine due to cavernous hemangioma or other conditions
What are the Different Types of Cystectomy?
The different types of cystectomy, depending on the procedure used, include the following:
Open cystectomy: In open cystectomy, the surgery is carried out through a lower midline incision of the abdomen.
Minimally invasive surgery: In minimally invasive surgery, the procedure is carried out through small incisions using special equipment. It includes:
- Laparoscopic cystectomy: which uses a tube with a camera at the lower end, called a laparoscope.
- Robotic cystectomy: where the procedure is carried out with the help of robotic arms, with the surgeon guiding them sitting at the console.
Minimal invasive surgery has the advantages of being associated with less blood loss, less pain, early healing, and better cosmetic effect on recovery (due to the absence of the long scar) as compared to open surgery. It however is costlier, requires surgeons trained in the procedure, and the operation takes a longer time.
Depending on the extent of the surgery, cystectomy can be classified as:
Radical cystectomy: In radical cystectomy, along with the urinary bladder, the prostate and seminal vesicles in men and the uterus, ovaries and part of the vagina in females are also removed. The intention of the procedure is to remove the entire cancer affecting the bladder to bring about a complete cure.
Partial cystectomy: In this procedure, only a part of the bladder is removed. Partial cystectomy may be done for localized bladder cancer, benign conditions (bladder diverticula), if the patient prefers and if the patient’s general condition precludes performance of radical surgery.
How should I Prepare before Cystectomy?
Tests done to diagnose your condition that needs cystectomy and to stage the cancer in case of bladder cancer will be reviewed by the surgeon. These may include:
- Examination of the urine sediment under microscope for presence of cancer cells
- Cystoscopy procedure (passing a thin tube through the urethra to visualize the interior of the bladder and obtain a sample of any abnormal or suspicious area for microscopy
- Imaging studies to determine the size and extent of the growth and presence of spread to local lymph nodes and distant sites
Routine tests: You will have to undergo routine tests before the procedure. Routine tests which are done before any surgery include:
- Blood tests like hemoglobin levels, blood group, and liver and kidney function tests
- Urine tests. Urine infection should be ruled out prior to the surgery with a urine culture if necessary
- Electrocardiogram (ECG) to study the electrical activity of the heart. In older patients, a detailed assessment of the heart may be required to make sure that they are fit for surgery
- Chest x-ray
Type of Anesthesia: Cystectomy is done under general or epdidural anesthesia. You will be asleep during the procedure and will not be aware of what is going on.
Pre-operative Check-up: Routine tests as indicated above are ordered a few days before the surgery. Medications like aspirin should be stopped around a week prior to the procedure. Patients are advised to stop smoking to ensure proper healing. Bowel preparation with the help of laxatives and a clear liquid diet may be advised a day or 2 before the surgery. Admission is required a day before the surgery.
The Day before Surgery: An enema is administered the previous afternoon or evening before the surgery along with gut-sensitive antibiotics.
Fasting before Surgery: Overnight fasting is required and occasionally intravenous fluid maybe required to keep you well hydrated. Sedation is sometimes required for good overnight sleep before the surgery.
Shift from the Ward or Room to the Waiting area in the Operating room: An hour or two before the surgery, you will be shifted to the operating room waiting area on a trolley. Once the surgical room is ready, you will be shifted to the operating room.
Anesthesia before Surgery: The anesthetist will inject drugs through an intravenous line and make you inhale some gases through a mask that will put you in deep sleep. Once you are asleep, a tube will be inserted into your mouth and windpipe to administer the anesthetic gases to overcome pain and keep you comfortable while the surgery is going on.
During the Cystectomy Procedure
During open radical cystectomy, once the anesthesia takes effect, your abdomen and the groin will be sterilized with antiseptics and draped to expose only the operation site. For the open surgery, you will lie on your back. A central midline incision will be made on your abdomen below the belly button. The underlying tissue and muscle will be separated. Blood vessels supplying the bladder will then be tied and cut. The bladder will then be separated from the urethra, the ureters and other neighboring tissues and delivered out. In men, the prostate, seminal vesicles and vas defers will also be removed while in women, the uterus along with the tubes, ovaries and the anterior part of the vagina will be removed. Pelvic lymph nodes are removed in both genders.
During laparoscopic radical cystectomy, you will be positioned with your legs separated and supported on stirrups. Pressure areas will be well padded and stockings will be used to prevent stagnation of blood in your legs. A small incision will be made below your belly button through which a cannula will be inserted. Carbon dioxide will be introduced into the abdomen through this cannula to inflate it so that the surgeon can visualize the inside of your abdomen clearly. Additional incisions will be made for the passage of instruments to carry out the surgery. Using the laparoscope and the instruments, the bladder will be separated from the surrounding structures and carefully removed. Pelvic lymph nodes are also removed. The urethra is removed if it is affected by the cancer.
During partial cystectomy, the diseased part of the bladder is removed and the defect is stitched up with absorbable sutures.
During robotic surgery, the surgeon sits at a console and controls robotic arms, which carry out the surgery with precision.
Urinary diversion:
The cystectomy procedure does not end with the removal of the bladder - it is also necessary to construct a passage for the urine to pass out of the body through a urinary diversion procedure. The methods used for urinary diversion include the following:
- Ileal conduit: A small part of the ileum or the small intestine will be obtained. It will be tied at one end and the other end will be attached to an opening in the abdomen (called stoma). The ureters will then be connected to the blind tube. Thus the urine that is formed in the kidneys will pass through the ureters into the ileal tube and later out of the body through the abdominal opening. Since the tube does not have any way to stop the continuous flow of urine, a bag has to be attached to the abdomen to collect the urine. The bag has to be emptied on a regular basis.
- Indiana pouch reservoir: In this procedure, the last part of the small intestine (the ileum), the beginning part of the large intestine and the cecum which is an enlargement at the junction of the two, will be used to make an internal pouch; the ureters will be attached to this pouch and the pouch will open out through the abdominal stoma. The urine from the internal pouch will have to be emptied on a regular basis with the help of a catheter. This procedure thus avoids the need of wearing an external bag.
- Orthotopic neobladder: This procedure also uses a part of the intestine, usually the ileum, to replace the bladder. The ureters will be attached on the upper side of the ileal pouch, the lower side of which will be attached to the urethra. However, this new bladder or ‘neobladder’ (‘orthotopic’ means that the part is grafted in a natural position) cannot completely replace the old bladder functionally. The bladder can be emptied by increasing the abdominal pressure by tightening the muscles, or through regular catheterization.
Once the surgery is complete, the incisions are closed, and a drain is left in the abdomen.
After Cystectomy Procedure
Waking up from General Anesthesia:. Once fully awake from anesthetic effect, you will be shifted on the trolley and taken to the recovery room.
Recovery room: In the recovery room, a nurse will monitor your vitals and observe you for an hour or two before shifting you to the room or a ward.
Post-operative recovery:
You may have to remain in the hospital for several days following the procedure.
- You will receive intravenous fluids and will be allowed to take in liquids once your bowel sounds return. You will be slowly shifted to semi-solid foods and later to solid foods.
- Chest physiotherapy may be started after 24 hours to prevent chest infection.
- The abdominal drain will be removed once the drainage is minimal.
- Prevention of deep vein thrombosis: Early movement of your legs and some mobilization prevents DVT or deep vein thrombosis, where a clot is formed in the deep veins of the legs with possible serious consequences
- Pain relievers and antibiotics may be prescribed.
Discharge from hospital:
- Once your wounds have healed and you can eat normal food, you will be discharged from the hospital.
- For partial cystectomy, catheter drainage of urine will be required for at least one week.
- You will be advised on how to take care of the stoma, the urinary bag and the catheter, and how to catheterize regularly. Repeated emptying may be required in the early days following the surgery, which can be reduced with time as the bladder capacity increases.
- You will have to restrict activities for six to eight weeks.
- You will have to follow up with your doctor on a regular basis, especially so if you had cancer to check for recurrence and to continue other forms of treatment like chemotherapy.
- In addition, you will have to be regularly monitored for proper function of the new urinary diversion created and for any complications that may arise.
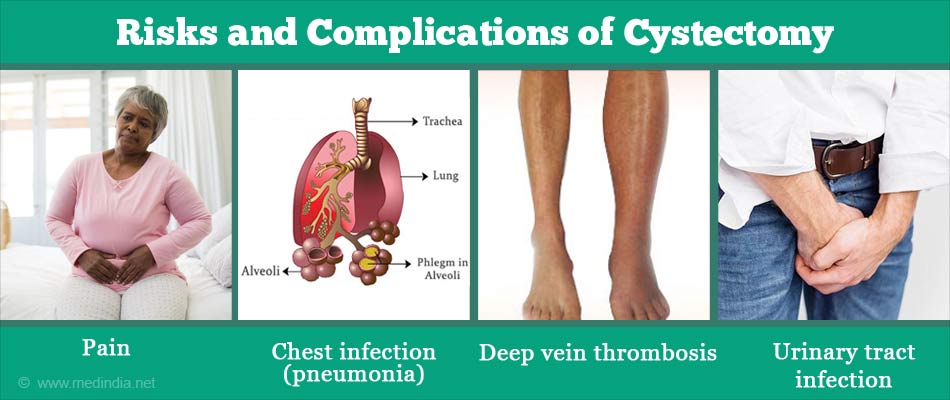
What are the Risks and Complications of Cystectomy?
Complications of cystectomy include the following:
Early complications:
- Infection, which can be prevented with postoperative antibiotics
- Pain, for which painkillers are prescribed
- Blood loss, which may even require blood transfusion
- Injury to the surrounding organs including the rectum
- Chest infection (pneumonia), - It can be prevented by administering painkillers, chest physiotherapy, and early mobilization
- Wound complications, which include infection and wound dehiscence due to improper healing
- Deep vein thrombosis, which can be prevented with early mobilization and low molecular weight heparin up to four weeks after cystectomy
- Leakage at the sites of the intestinal surgery, or through the pouch at suture lines.
- Postoperative ileus, where the intestines fail to move following the surgery.
- Impotence in males, which can be avoided with a nerve-sparing surgery when possible. Females may suffer from sexual difficulties like problems with sexual arousal and ability to have an orgasm following nerve damage.
- Early menopause occurs in young women who have undergone radical cystectomy.
- Complications related to anesthesia
Late complications:
- Urinary tract infection, which can be detected on urine routine and culture tests. Incisional hernia, which is an outpouching of the inner lining of the abdomen through the weak point of the incision.
- Voiding difficulties in orthotopic neobladder, which may result in urinary retention or incontinence. Urinary retention is usually relieved with catheterization. Incontinence improves with time, but a pad may be required. Severe incontinence may be treated with medications, collagen injection around the urethra, a urethral sling introduced surgically to support the urethra, or an artificial urinary sphincter
- Deterioration in renal function could occur due to various causes requiring appropriate treatment as indicated
- Inflammation and narrowing of the urine outlet (stoma) created.
- Stone formation in the bladder, which may be removed by endoscopic procedure (via a tube introduced into the bladder).
- Bowel obstruction, due to adhesions formed due to the surgery and may need repeat surgery.
- Recurrence of the cancer, which will be treated appropriately
- The quality of life can be affected following the diversion surgery. The cost implications also have to be kept in mind.