What is Endoscopic Retrograde Cholangio-Pancreatography?
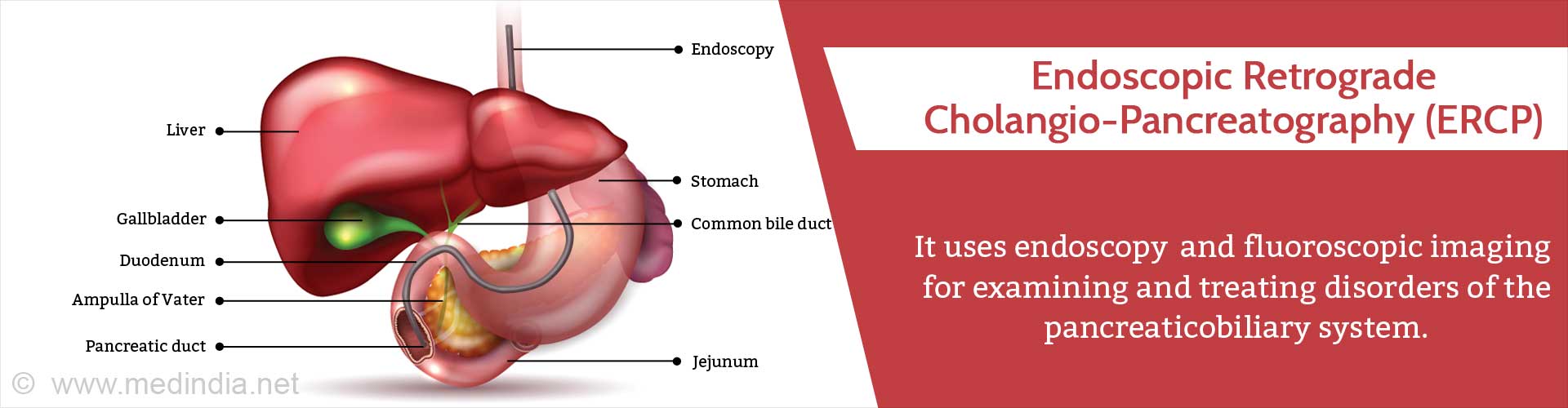
Endoscopic retrograde cholangiopancreatography (ERCP) is an investigative technique which uses endoscopy and fluoroscopic imaging for the diagnosis and treatment of disorders of the biliary and pancreatic systems. In this procedure, a thin, flexible, telescopic instrument, called an endoscope is passed through the mouth and stomach to the duodenum for treating diseases of the gallbladder, biliary system and the pancreas.
When it was first introduced in the 1970s, ERCP was primarily used as a diagnostic tool. However, with the advent of less invasive and safer diagnostic procedures, such as endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP), ERCP has now essentially become a therapeutic tool.
The digestive tract includes the mouth, food pipe and stomach which leads to the small intestine, large intestine and rectum. The liver and pancreas form digestive juices and pour it through duct into the first part of the small intestine called the duodenum. The common hepatic duct from the liver joins the cystic duct from the gallbladder to form the common bile duct. This duct joins the pancreatic duct to form the ampulla of Vater which opens in the duodenum. The endoscope is passed till this region during ERCP.
What are the Reasons to do ERCP / Indications for ERCP?
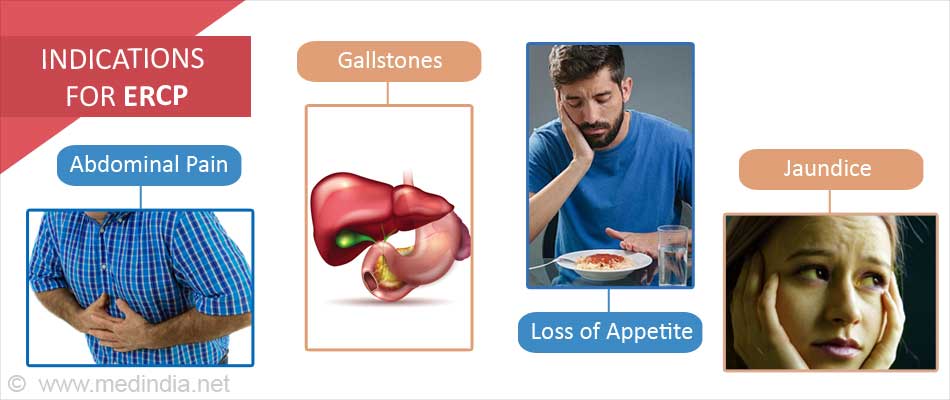
The liver, gallbladder, pancreas, bile ducts and the major duodenal papilla or ampulla of Vater can be involved in many diseases with numerous symptoms. The major reasons for doing an ERCP include the following:
- Obstruction of the bile duct by gallstones, strictures, or compression by tumors.
- Persistent or recurrent abdominal pain that cannot be properly investigated by other diagnostic modalities.
- Jaundice, which occurs due to blockage of the bile duct.
- Unexpected loss of appetite resulting in weight loss.
- Confirmation of pancreatic or bile duct cancer by obtaining biopsy samples, so that surgery or other treatments can be instituted.
- Confirmation of sphincter of Oddi dysfunction.
Since there are significant complications associated with ERCP, the doctor must carefully weigh the risks versus benefits of the procedure. Here lies the importance of the various indications before proceeding with the procedure.
How do you Prepare before ERCP?
You will undergo a blood test before the procedure, either on the previous day or on the day of the procedure. You should be on an empty stomach and should not have eaten after midnight preceding the day of the procedure. If the procedure is scheduled for later in the day, you should not eat for at least 6-8 hours prior to the procedure. Drinking of water or other clear liquids should be stopped at least 4 hours before the procedure. In case any medicines are required to be taken, such as for heart ailments, blood pressure and diabetes, these should be consumed with minimal amount of water in the early morning, subject to the doctor’s approval.
Medicines that should be avoided before the procedure or require adjustment of the dosage and timing, include the following:
- Aspirin
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Insulin
- Antacids
The doctor should be informed regarding the following:
- If you are on blood thinners (anticoagulants) such as heparin, warfarin, or clopidogrel.
- If you underwent a CT scan or barium X-ray in the preceding 2-3 days.
- In case of pregnancy.
- In case of any allergy. Allergy to iodine is particularly important as the contrast dye used in the procedure contains iodine.
On the day of the ERCP, the doctor or nurse will explain the procedure and answer any questions, following which an informed consent form will need to be signed.
What Happens During the Procedure?
You will be asked to remove dentures, spectacles, contact lenses, and hearing aids, as applicable. A local anesthetic will be sprayed at the back of your throat to numb the area, as the endoscope will be inserted through the throat. Small monitoring devices will be placed on the skin to measure the pulse, blood pressure and blood oxygen levels.
A plastic guard will be placed in your mouth to protect the teeth. Then a sedative-analgesic such as droperidol, diazepam, midazolam, or meperidine will be administered through an intravenous (IV) channel to make you relaxed and sleepy.
During the procedure, an endoscope is passed through the mouth, food pipe and stomach, into the duodenum. The endoscope is fitted with optical fibers through which light can illuminate the relevant parts of the gastrointestinal (GI) tract being investigated. X-ray pictures of the bile and pancreatic ducts are taken (technically termed as cholangiopancreatography) using an instant X-ray machine called a fluoroscope.
Since the ducts do not show-up clearly in ordinary radiographs, a contrast dye is injected, which appreciably increases the visibility of the ducts. The contrast dye is injected into the papilla of the duodenum and flows backwards up the pancreatic and biliary ducts. For this reason, the injection is called a “retrograde” injection, which is done via a narrow plastic tube that protrudes through the side of the endoscope. The X-ray pictures are then taken.
After a definitive diagnosis is made, any one of the following endoscopic techniques is used as a therapeutic intervention:
- Sphincterotomy: This is a surgical procedure which uses the endoscope to cut the muscle surrounding the opening of the common bile duct or pancreatic duct and remove gallstones and other obstructions.
- Stenting: This procedure is used to open-up obstructed bile or pancreatic ducts by inserting a stent at the site of blockage. Stenting can be used to treat biliary or pancreatic duct leaks, as well as following stricture dilation to keep the duct open.
- Endoscopic Stone Extraction: Endoscopy can be used to remove gallstones from the common bile duct, as well as stones lodged in the pancreatic duct.
What are the Advantages and Disadvantages of ERCP?
A major advantage of ERCP is that it provides detailed and accurate information about the pancreaticobiliary system that is difficult to diagnose by EUS. It also provides a less invasive procedure than open surgery for treating several pancreatic diseases.
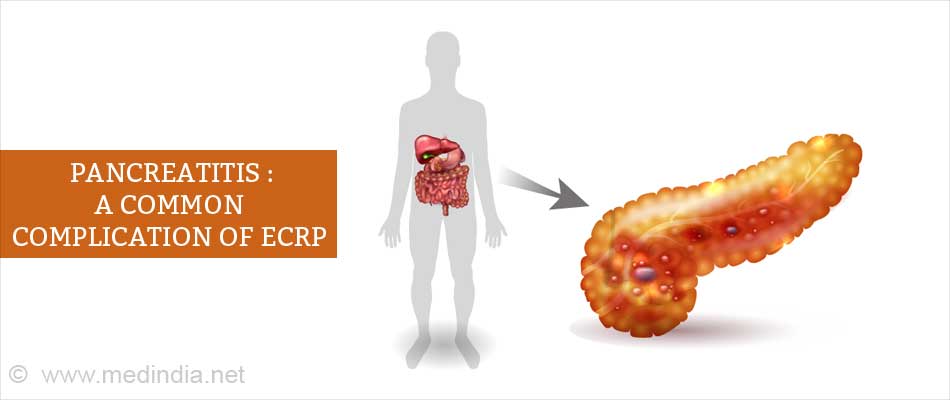
A major disadvantage of ERCP is the risk of occurrence of complications. This usually occurs in 5-20% of patients and can vary with the patient, disease, and the type of ERCP procedure and the treatment modality. Some of the following complications may occur:
- Pancreatitis: This is the most common complication that occurs in ~10% of patients undergoing ERCP and requires hospitalization.
- Bleeding: This can occur during sphincterotomy, but can usually be controlled by the surgeon during the ERCP procedure.
- Intestinal Perforation: This can be caused by the endoscope itself while performing sphincterotomy. The perforation requires surgical intervention to repair.
- Infection: This can occur in the biliary and pancreatic ducts following ERCP, especially if an obstruction is present that cannot be cleared by the ERCP procedure. Treatment usually involves antibiotics, but may require surgery to clear the obstruction.
Management after ERCP
After the procedure, you will be transferred to the recovery room where it will take approximately 1-2 hours for the effect of the medications to wear off. During this period, you will be under observation for any complications that may arise as a result of the procedure. ERCP is usually performed as an outpatient procedure and you will be discharged the same day. In case of any complications, you may need to be admitted overnight for further observation.
Upon discharge, you must be accompanied by a family member and must not drive due to the residual effects of the sedatives used in the procedure. At home, you should take adequate rest and only have a light meal and plenty of fluids. The routine medications can be restarted, unless instructed by the doctor not to do so. During the recovery period, you should be alert about early signs of complications. These include the following:
- Abdominal pain
- Fever
- Dizziness
- Nausea
- Vomiting
- Yellowing of the skin and white of the eyes
- Black colored stool
- Bleeding from the rectum
Health Tips
- Eat high-fiber diet: A diet high in fiber and rich in whole grains, vegetables, legumes, and fruits can improve digestive health.
- Limit your intake of foods high in fat: Fatty foods tend to slow-down the digestive process, thereby increasing the chances of constipation. However, since fats are necessary for the body, limited amounts of fat should be consumed in combination with dietary fibers.
- Eat lean meats: Proteins are an essential component of a healthy diet. But fatty meats can cause digestive problems, so it is better to go for lean meat such as the mutton from the thighs, pork loin, and skinless poultry.
- Add probiotics to your diet: Probiotics are good bacteria that are naturally present in the gut. These help to fight the effects of a poor diet by enhancing the absorption of nutrients and boosting the immune system. Good sources of probiotics include low-fat yogurt and kefir.
- Take meals at fixed times: Consumption of meals such as breakfast, lunch, dinner and snacks at fixed times helps to keep the digestive system in good condition.