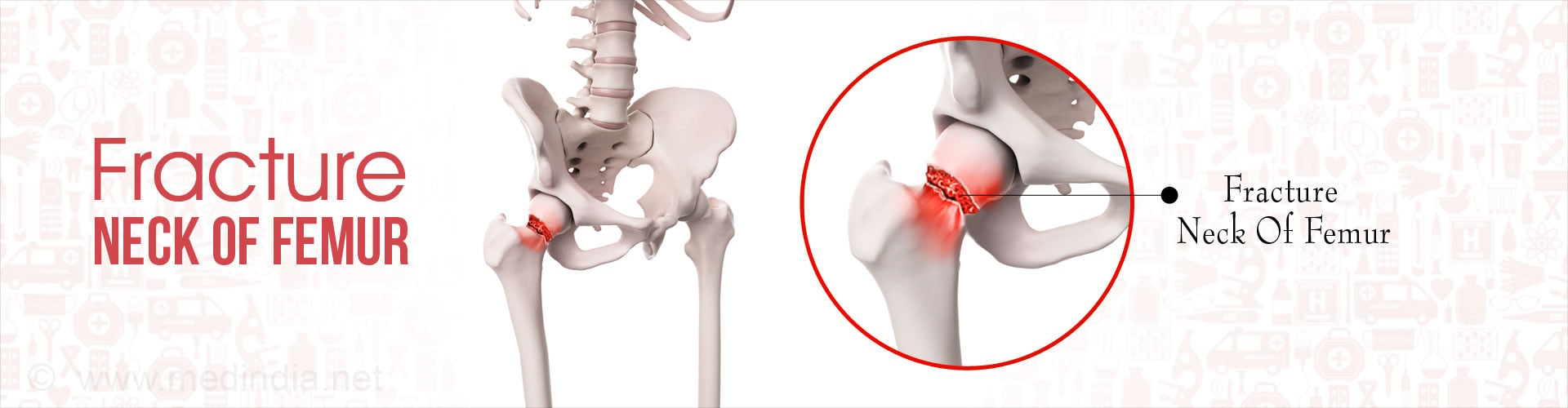
What is a Femoral Neck Fracture?
Fracture neck of femur is a type of hip fracture seen in elderly people. An unsteady gait or reduced bone mineral density, both of which may be seen in the elderly is a predisposing factor. Elderly, osteoporotic women are particularly at risk.
Incidence and Risk Factors
90% occur to those over the age of fifty. In the US alone, 250,000 hip fractures occur annually, and this figure is expected to double by 2040.
Risk doubles every decade after fifty. These include the following
- Osteoporosis
- Female sex, and increased age
- Excessive coffee or alcohol consumption
- Smoking
- Dementia
- Defective vision
- Physical inactivity
- Arthritis
- Low BMI
- Living in an institution
Types of Femoral Neck Fracture
Femoral neck fractures are a type of proximal hip fractures (occurring proximal to the inter-trochanteric line). All proximal fractures are intracapsular fractures. They can be subdivided into
- Subcapital – occurring at junction of femoral head and neck
- Transcervical – midportion of femoral neck
- Basicervical – base of femoral neck
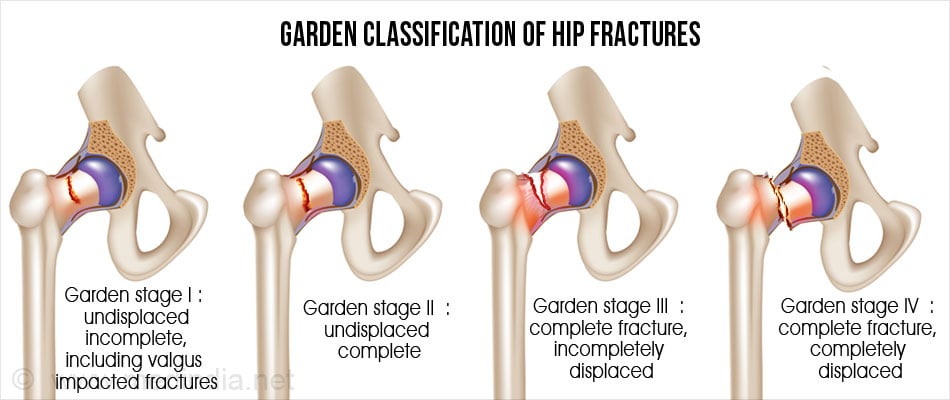
Additionally, the severity of a subcapital fracture is graded according to the Garden
Classification of hip fractures as follows:
- Garden stage I : undisplaced incomplete, including valgus impacted fractures.
- Garden stage II : undisplaced complete
- Garden stage III : complete fracture, incompletely displaced
- Garden stage IV : complete fracture, completely displaced
Causes of a Femoral Neck Fracture
Falls account for > 90% of cases in persons over 50 years. It usually affects elderly people who have weak bones. It is common occurrence with the first snowfall of the season.
- High impact activities in younger individuals leading to stress fracture
- Pathologic fracture may occur at any age, including secondary deposit of malignancy, hyperparathyroidism, osteogenesis imperfecta, steroids, Pagets disease, and infection
Signs and Symptoms Of A Femoral Neck Fracture
- Severe pain in hip or groin
- Difficulty in movement immediately after a fall
- Inability to bear weight on the leg on the side of injury
- Stiffness, bruising and swelling in and around your hip area
- Limb shorter on the side of injury
- Rest the fractured leg in an outward direction
Stress fracture, especially in younger individuals may not have a history of fall or trauma. The following points need to be noted in the history.
- Participation in repetitive cyclic activity
- Recent change in activity or equipment
- Atraumatic history
- Pain with weight bearing
- Relief of pain with rest
- Menstrual irregularities
- Predisposing osteopenia
- Insidious onset of pain
Complications of Femoral Neck Fracture
About half of people with a hip fracture don’t regain their ability to live independently. In the absence of surgical intervention, there is increased risk of
- Avascular necrosis of femoral head
- Non-union
Prolonged immobility following the fracture may increase the risk of the following
- Blood clots in legs or lungs
- Occurrence of bedsores
- Urinary tract infection
- Lung infections
- Further loss of muscle mass, increasing risk of falls and injury
Any hip fracture restricts future independence and may even shorten one’s life.
Diagnosis of a Femoral Neck Fracture
Diagnostic imaging is central to the diagnosis of femoral neck fractures. These include
1. Plain x-ray hip
Helps to rule out any obvious fractures and also determine the site and extent of the fracture. However, a plain radiograph may appear normal in a patient with a femoral neck stress fracture or an undisplaced fracture.

2. Magnetic Resonance Imaging (MRI) hip
If pain persists in the presence of a normal Plain x-ray, an MRI may be done to rule out a hairline or an occult fracture.
3. Bone scanning
Bone scans may be indicated when a stress fracture, tumor, or infection is suspected.
Treatment of a Femoral Neck Fracture
Acute Phase
Treatment of hip fracture generally involves a combination of surgery, rehabilitation and drugs. Several factors need to be considered before a treatment plan is recommended
The aim of treatment in patients with femoral neck fractures threefold, namely - to promote healing, prevention of complications, and return of normal function.
1. Physical therapy
- In uncomplicated fractures, especially those in younger athletes, treatment must focus on rest and reversal of any training errors. Modifying one's risk factors is critical at this point to prevent progression of the fracture.
- A physical therapist may be necessary to reinforce the physician's instructions for rest and helping the patient modify his or her training program to allow healing.
- For fitness, the remaining extremities may be exercised. There should be no weight bearing on the affected hip, and suitable strengthening exercises may be prescribed that avoid weight bearing.
- He can evaluate the patient for gait or anatomic abnormalities that may have caused the fracture. A few patients may require to be fitted with an external device to control excessive pronation that may lead to increased stress on the femoral neck and increase risk of fracture.
- Whether surgery is indicated or not, the physical therapist helps in educating the patient and prescribing suitable exercises.

2. Surgical Management
The choice of surgery generally depends on the site and severity of the fracture, whether the broken fragments retain their alignment or not (displaced fracture), age, and any underlying health conditions.
- Nondisplaced femoral neck fractures have to be initially treated with complete non–weight-bearing ambulation with using crutches. Plain x-rays needs to be taken every 2 – 3 days to monitor the progress. If pain does not lessen or there is evidence of fracture line expansion, internal fixation with multiple parallel lag screws or pins is indicated.
- Displaced fractures - Management of displaced femoral fractures depends on the age and mobility of the patient.
- A displaced fracture in a young patient is considered an orthopedic emergency. Early open reduction and internal fixation is considered the treatment of choice. The chances of returning to a high level of sport participation is poor.
- In elderly patients with displaced fracture, treatment options include open reduction and internal fixation or prosthetic replacement. The choice is made depending on the mobility, degree of independence and cognition of the patient.
- In general, hip replacement surgery is considered the better option in an elderly patient with fairly good mobility prior to surgery and good cognition. The replacement is said to be complete when the acetabulum, and femoral head and neck are all replaced and termed partial if the head and neck alone are replaced.
- Neither treatment may offer much benefit in patients with severe cognitive impairment.
- Tension fractures are potentially unstable and may require operative management. On the other hand, compression fractures tend to be stable and can be managed non-operatively.

3. Medications
In the initial stages, pain relief is important. Very often, acetaminophen or an NSAID is given. Occasionally opiates may be necessary for more severe pain.
A small percentage of patients may have a risk of a future fracture. Biphosphonates may help reduce that risk of osteoporosis.
Bisphosphonates generally are contraindicated in people with kidney problems. Occasionally, long-term therapy may cause pain and swelling in the jaw, visual defects or an atypical hip fracture.
Recovery and Maintenance Phase
For young active persons, especially athletes, Rehabilitation Program continues into the recovery and maintenance phases.
Fitness and muscle strengthening exercises are prescribed. It is important to maintain aerobic conditioning throughout. Gradual weight bearing on the injured side is introduced.
Patients are generally permitted to return to running or aquatic sports; but, contact sports are restricted.
After discharge, elderly patients need to work with an occupational therapist to learn techniques for becoming independent in day to day activities, such as using the toilet, bathing, dressing and cooking. The occupational therapist will determine if a walker or wheelchair is necessary to help regain mobility and independence.
Prognosis of Femoral Neck Fracture
Prognosis is variable. In the elderly, return to pre-fracture levels of mobility is hardly achieved. Their independence is restricted and mortality rates are also be increased. Because of unsteady gait such individuals are also at risk of future falls and fracture.
Active young persons and athletes may not be able to return to pre-morbid levels of fitness or level of competition.
The prognosis is better in stable and undisplaced fractures.
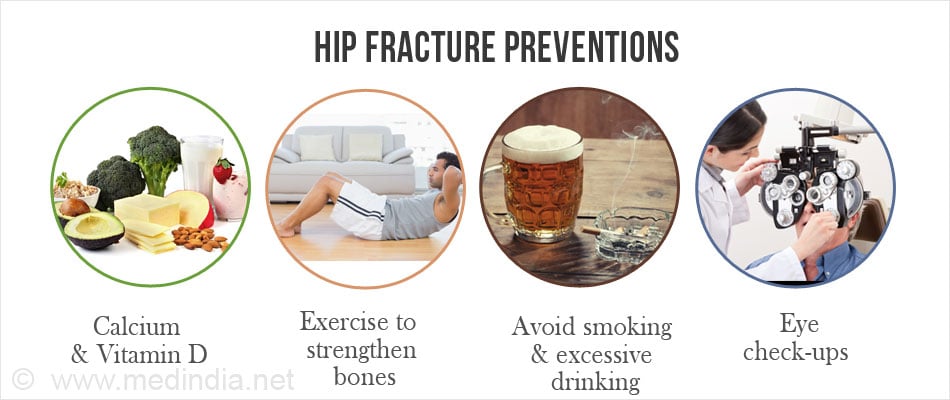
Prevention of Hip Fracture
Hip fractures can be largely prevented by following certain precautions to avoid falls and bone strengthening measures. These include the following
- Calcium and Vitamin D – Men and women over 50 years should take 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Exercise to strengthen bones and improve balance – Help in reducing risk of falls.
- Avoid smoking and excessive drinking – May reduce bone density. Alcohol may increase the risk of falls by causing impairment of gait.
- Making the house fall proof – Removal of rugs on the floor that are not stable. Keeping furniture out of the way to avoid falling. Put anti-skid mats and hand rail in the toilets and avoid wet floors.
- Eye check-ups – Should be done periodically .
- Side effects of medications – Need to discuss the medications being taken to see if any of them are increasing the risk of falls by causing say dizziness or weakness.
- Using a walking stick or a walker – Especially if the gait is unsteady.
- Getting up slowly from seated position – To avoid feeling dizzy.