What is Gastrectomy?
Gastrectomy is a surgical procedure where a part of or the complete stomach is surgically removed. It may be done as an open surgical procedure or through laparoscopy.
While living without a stomach appears absurd, it is not impossible. Diet alterations will be required to avoid the feeling of discomfort and immediate fullness. It should also be remembered that in many gastrectomy surgeries, the full stomach is not removed but a small section is left behind.
Anatomy of the Stomach
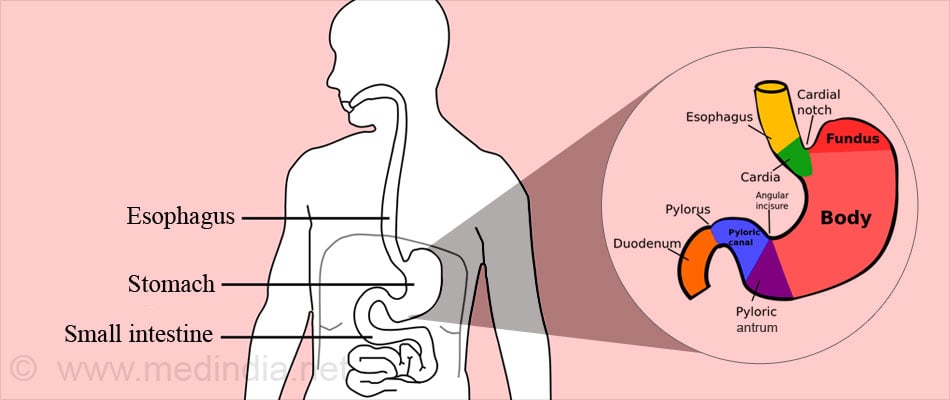
The stomach is a muscular ‘Curved sack that is J & bean shaped.’ It is located on the left side in the upper abdomen behind the ribs and is the widest section of the digestive tract. Its capacity varies but on an average can hold from 1 to 2 liters. When fully distended it can hold up to 4 liters of food in some individuals. The stomach connects the food pipe and the small intestine.
The upper end of the stomach is called cardia while the lower end is the pylorus. These are guarded by the cardiac sphincter and the pyloric sphincter, respectively. The sphincters close at both ends once the stomach is filled for the digestion process to take place.
The part of the stomach that extends upwards beyond its junction with the food pipe is called the fundus. The body of the stomach extends between the fundus and the pyloric canal and has the upper lesser curvature and the lower great curvature. A tissue called the lesser omentum is attached at the lesser curvature while the greater omentum is attached along the greater curvature. Blood vessels, nerves and lymph nodes supplying and draining the stomach pass through the omenta to reach the stomach.
Functions of Stomach – The stomach functions as a reservoir for food and also the section where the food literally gets sterilized and partly digested. The stomach secretes hydrochloric acid that has a pH between 1.5 to 3. This acidic secretion ensures that all microbes are killed or inactivated and makes sure that they don’t enter or attack our body.
The stomach lining is protected from strong acid by a mucus secretion, the lining keeps getting changed almost every 2 weeks.
The stomach digests the food especially proteins by breaking them down into smaller chain amino acids. It mixes the food via the peristaltic slow movements with other secretions besides the acid. It also produces a factor that helps in ingestion of vitamin12 and prevents anemia.
Why is Gastrectomy Done?
Gastrectomy is done for the following conditions:
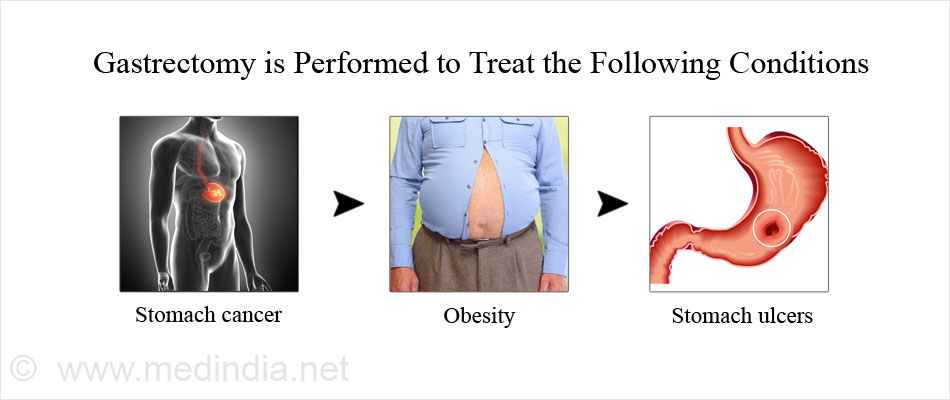
- Stomach Cancer: Partial or total gastrectomy is done for stomach cancer depending on the extent of the disease. The most common type of stomach cancer is called adenocarcinoma. The patient may complain of symptoms like weight loss, coughing up of blood, black stools and stomach discomfort.
Sometimes the symptoms are so subtle or minimal that only once the tumor has reached a very advanced stage that it produces symptoms that are noticeable.
- Obesity: Surgery is done to treat obesity is called bariatric surgery. Patients who are usually considered for bariatric surgery include those with a body mass index (BMI) higher than 40 kg/m2 or a BMI higher than 35 kg/m2 in the presence of other high-risk comorbid conditions such as sleep apnea, Pickwickian syndrome, diabetes mellitus, or degenerative joint disease.
- Stomach Ulcers: Stomach ulcers are often a consequence of increased acidity, H pylori infection or intake of non-steroidal painkillers. The patient experiences a burning sensation in the upper abdomen especially when hungry. Stomach ulcers are usually treated with medications. Ulcers that bleed or do not respond to medications may require surgery.
What are the Types of Gastrectomy?
Depending on the type of surgical procedure, gastrectomy may be classified as:
- Open gastrectomy, which is an open surgical procedure
- Laparoscopic gastrectomy, which is a keyhole surgery. It is done with the help of small diameter (about a cm or less) long telescopic instrument that is introduced into the abdomen through small key-hole opening.
Carbon dioxide or air is insufflated into the abdomen for easy visualization. Surgical instruments are introduced through trocars inserted through additional small openings. Though the surgery results in lesser postoperative pain and quicker recovery, it takes longer time and can be done only for selected cases that require gastrectomy.
Depending on the extent of the gastrectomy, the gastrectomy may be classified as:
- Total gastrectomy: In total gastrectomy, the complete stomach is removed along with surrounding structures which may include lymph nodes and the spleen. The extent of the surgery depends on the spread of the disease condition to the surrounding structures.
- Partial gastrectomy: Partial gastrectomy is a surgical procedure where a part of the stomach is removed. Depending on the amount of stomach resected, partial gastrectomy may be classified as:
- Antrectomy, where 30% of the lower stomach is resected
- Hemigastrectomy, where half the stomach is resected
- Subtotal gastrectomy, where around 80% of the stomach is resected
- Following partial gastrectomy, the continuity of the digestive tract is maintained using procedures like the following:
- Billroth I partial gastrectomy: In this surgery, the remaining part of the stomach is connected to the duodenum, i.e. the first part of the small intestine
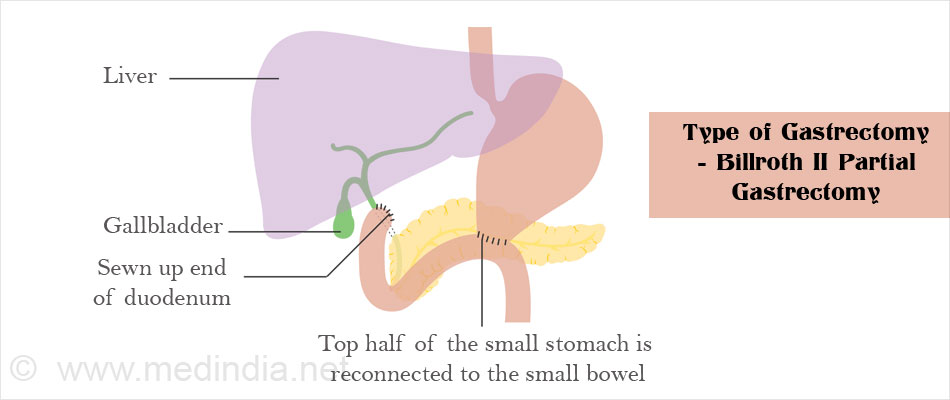
- Billroth II partial gastrectomy: In this surgery, the remaining part of the stomach is connected with an opening made in the wall of the second part of the intestine called the jejunum, while the upper end of the duodenum is converted into a stump
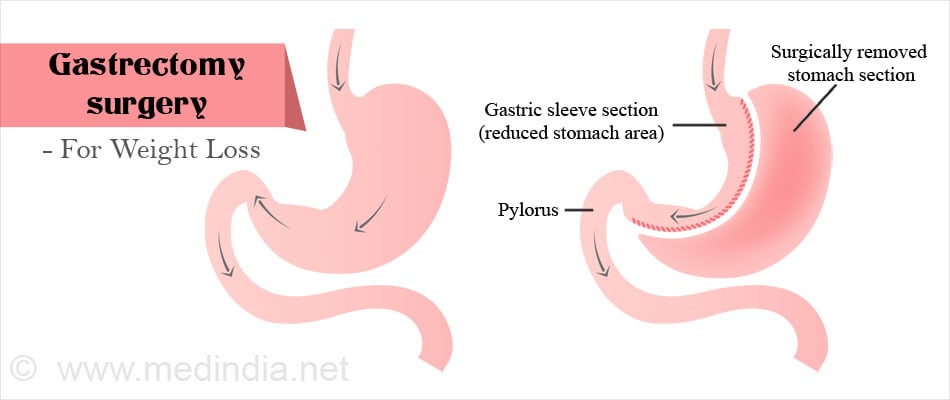
- Sleeve or longitudinal gastrectomy or vertical sleeve gastrectomy. This procedure is performed to treat morbid obesity. In this procedure, a longitudinal strip of the stomach is removed and the stomach is converted into a tube-shaped structure. The cut ends are closed with staples. Thus, the volume or capacity of the stomach is reduced. The secretion of hormones by the stomach is also reduced, resulting in loss of appetite, which is further beneficial not only for treating obesity but also helps in controlling diabetes better.
What are the Tests Done Before a Gastrectomy Procedure?
Tests done before a gastrectomy procedure include the following:
- Routine tests: Routine tests which are done before any surgery include:
- Blood tests like hemoglobin levels, blood group, and liver and kidney function tests
- Urine tests
- ECG to study the electrical activity of the heart
- Chest x-ray
- In older patients, a detailed assessment of the heart may be required to make sure that they are fit for surgery.
- Tests to evaluate the stomach pathology: Tests to diagnose the stomach disease and the extent of the disease include the following:
- Upper (Gastro-duodenal) endoscopy: Upper endoscopy is an office procedure where a tube with a small camera is inserted through the mouth into the stomach to study its inner lining, along with the lining of the food pipe and the first part of the small intestine. A biopsy of the abnormal tissue may be obtained and subjected to pathological testing.
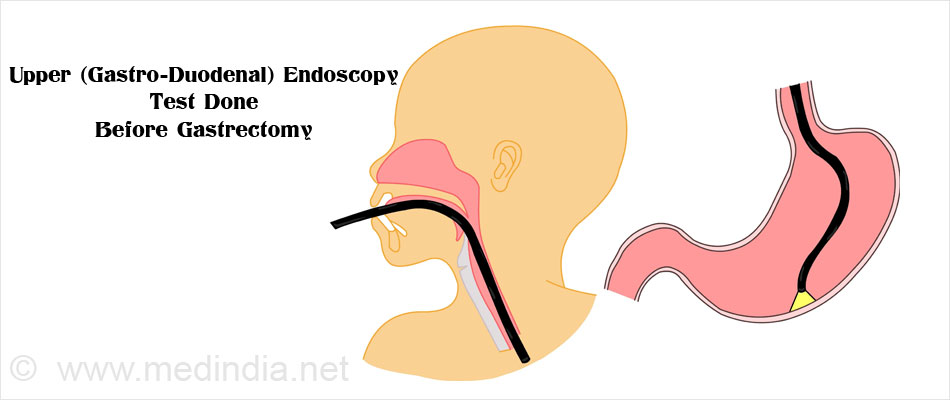
Endoscopic ultrasound may also be done to study the extent of the stomach cancer if present.
- CT scan: A CT scan is a radiological test that obtains images at different angles. It helps to evaluate the pathology as well as its spread into the abdomen. Contrast material is sometimes injected into the vein to obtain better images.
How is Gastrectomy Performed?
Type of Anesthesia - Gastrectomy is done under general anesthesia. You will be asleep during the procedure and will not be aware of what is going on.
Pre-operative Check-up - Routine tests as indicated above are ordered a few days before the surgery. Admission is required usually a day before the surgery.
Day before Surgery - An enema maybe administered the previous evening or night before the surgery.
Fasting before Surgery - Overnight fasting is required and occasionally intravenous fluid maybe required to keep you well hydrated. Sedation is sometimes required for good overnight sleep before the surgery. A pre-operative intravenous broad spectrum maybe prescribed after checking for any allergies.
Shift from the Ward or Room to the Waiting area in the Operating room - An hour or two before the surgery, you will be shifted to the operating room waiting area on a trolley. Once the surgical room is ready, you will be shifted to the operating room.
Shift to the Operating room - The ambience in the operating room can sometimes create anxiety within you and a small amount of sedation can help overcome it.
From the trolley, you will be shifted on to the operating table. As you look up, you will see the operating light console and at the head-end will be the anesthesia machine. There may also be monitors to check oxygen levels, ECG and other vital parameters. A constant beeping sound may be heard from the monitors, which may sometimes be irritating. You may also see instrument trolleys and a few operation theatre staff dressed and masked doing the final checks before the surgery starts.
Anesthesia before Surgery – During the anesthesia, the anesthetist will inject drugs through an intravenous line and make you inhale gases through a mask that will put you in deep sleep. Once you are asleep, a tube will be inserted into your mouth and windpipe to administer the anesthesic gases to overcome pain and keep you comfortable while the surgery is going on.
Gastrectomy Procedure
Prior to the gastrectomy procedure, a tube called the nasogastric tube is inserted into the stomach via the nose to empty the stomach contents. A catheter is introduced into the urinary ladder to monitor the urine output.
For an open surgery: The incision is made extending from upper mid-abdomen to the belly button. The stomach is exposed and separated from the tissues attached to it.
The abdomen is carefully examined and other organs that may also be affected like liver, mesentery, intestines are also checked for any spread of the disease.
The supplying arteries are separated carefully to avoid excessive bleeding. The diseased part of the stomach or the whole stomach is then cut out, depending on whether the procedure is partial gastrectomy or total gastrectomy. Lymph nodes are examined and diseased nodes are dissected out.
The cut ends of the digestive tract are reattached. The remaining part of the stomach is attached either to the duodenum or the jejunum. Once the surgery is complete, the abdominal incision is closed with sutures and an abdominal drain is left in place.
Laparoscopic or Robotic surgery - Is also sometimes used for gastrectomy procedure.
The steps for laparoscopic surgery are similar to open surgery. Most bariatric surgeries are performed using a laparoscope.
In robotic surgery the surgeon controls robotic arms remotely and carries out the surgery with precision.
In the sleeve procedure, a longitudinal section of the stomach is stapled off. The stapled line may be strengthened to prevent leakage.
Waking up from General Anesthesia – If you have received general anesthesia, once the surgery is over, you will wake up and the tube down the wind pipe will be removed. You will be asked to open your eyes before the tube is removed. You will be sedated and the voice of the anesthetist may be faint. Once the tube is out, you may have cough and sometimes nausea.
You may still have the nasogastric tube and the urinary catheter. There will also be an intravenous line. You will remain on oxygen. Once fully awake, you will be shifted on the trolley and taken to the recovery room.
Recovery room – In the recovery room, a nurse will monitor your vitals and observe you for an hour or two before shifting you to the room or a ward.
Post-operative recovery – You will remain in the hospital for several days following an open procedure. You will receive intravenous fluids and will be allowed to take in liquids once your bowel sounds return, which may be two to three days following the surgery. You will be slowly shifted to semi-solid foods and later to solid foods.
Chest physiotherapy may be started after 24 hours to prevent chest infection.
After laparoscopic or robotic surgery, you maybe discharged after a day or two. However it is best to only get discharged after your bowel functions have returned and you are mobile.
DVT Prophylaxis – Early movement of your legs and some mobilization prevents DVT or deep vein thrombosis, where a clot is formed in the deep veins of the legs. The clot can travel up to the lungs and even be fatal. Other measures like small dose of heparin and special stockings may also be used.
Pain relievers may be prescribed depending on the extent of the pain.
Discharge from hospital – Once your wounds have healed and you can eat normal food, you will be discharged from the hospital. You will receive instructions regarding the type of diet you should follow.
What are the Surgical Complications and Risks of Gastrectomy Surgery?
Complications of gastrectomy include the following:
- Excessive bleeding may require another surgery
- Wound infection
- Injury to the surrounding structures during the surgery like the spleen, gallbladder and intestine
- Leakage from the staple line
- Post-operative pain
- Deficiency of nutrients like vitamin B12, calcium, vitamin D and iron, resulting in conditions like anemia and osteoporosis
- Diarrhea

- Weight loss. This side effect is desirable in patients undergoing bariatric surgery
- Reflux of stomach contents into the food pipe resulting in symptoms of heartburn
- Postprandial dumping syndrome. Due to the absence of the stomach or reduction in stomach volume following gastrectomy, the hypertonic contents of the stomach get dumped into the intestine. These contents pull in water from the body into the intestinal lumen resulting in symptoms of abdominal pain, diarrhea, flushing and dizziness. The symptoms subside on emptying the bowels. Dumping syndrome can be avoided by a proper control on the diet.
What are the Dietary Modifications to be Followed Post-Gastrectomy?
Several dietary modifications are advised post-gastrectomy surgery. These include:
- Small amounts of food should be taken at frequent intervals
- The food should be high in protein and low in carbohydrates. Simple sugars should be avoided
- Water should be avoided along with or immediately after eating
- People in whom the upper end of the stomach is surgically removed should sit up for at least one hour after meals to prevent reflux
- Vitamin B12, vitamin D and other supplements may be needed following the gastrectomy procedure