What is Hemorrhoidectomy?
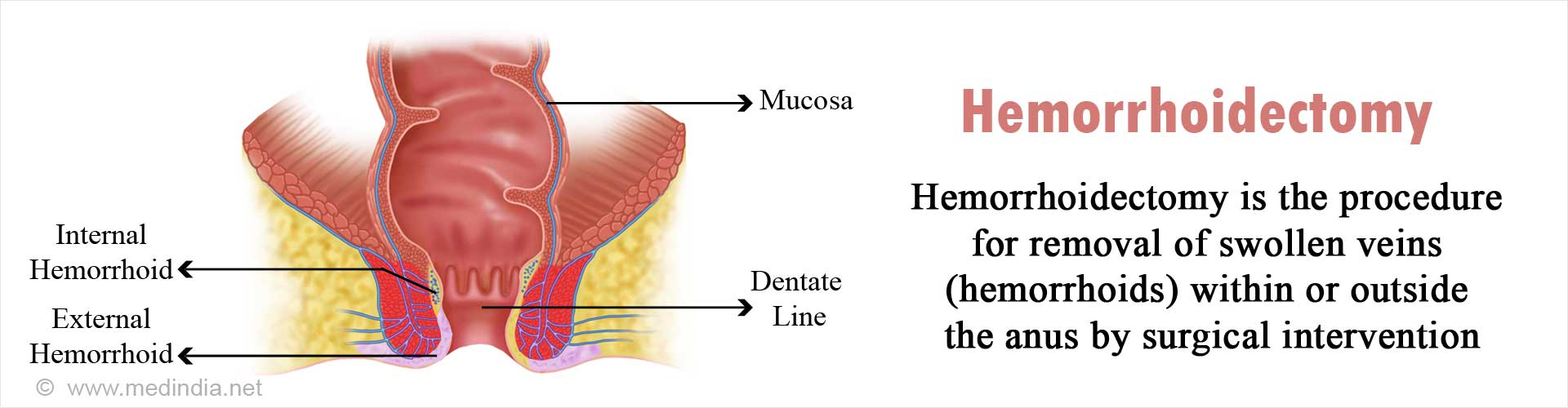
Hemorrhoidectomy is a surgical procedure in which the external or internal hemorrhoids are removed. Surgical hemorrhoidectomy is the best treatment option for hemorrhoids, with a success rate of 95%.
Hemorrhoids, also known as piles is an enlarged, swollen aggregation of inflamed veins along with smooth muscle and connective tissue in the rectum and anus that can cause discomfort and bleeding. Sometimes, the hemorrhoid may protrude outside the anus (external hemorrhoids) or remain within the rectum (internal hemorrhoids). In India, over 40 million people suffer from hemorrhoids. Approximately 1 million new cases are reported annually, 47 per 1000, with the incidence increasing with age. The usually affected age group is 45-65 years.
Why is Hemorrhoidectomy done?
Symptomatic hemorrhoids that affects the quality of life is an indication for intervention. The symptoms include pain, bleeding and difficulty maintaining anal hygiene. The main purpose of a hemorrhoidectomy is to relieve the symptoms such as pain and bleeding in cases that have not responded adequately to conservative treatment. Hemorrhoids is usually managed by diet and medicines, since this is not a life-threatening condition. Surgery is generally recommended only as a last resort, when all else fails. Hemorrhoidectomy is particularly useful for treating large internal hemorrhoids, which can cause complications, such as mucus discharge or fecal leakage as the internal hemorrhoids prolapse through the anal canal. The accompanying irritation of the perianal skin can result in severe itching (pruritus). External hemorrhoids can also be a cause of great discomfort.
How do you Prepare Before a Hemorrhoidectomy?
Hemorrhoids first comes to the notice of the doctor when a patient complains of bleeding following a bowel movement. The doctor performs a digital examination of the rectum in order to rule out other possible causes. Following the digital examination, the rectum and lower part of the large intestine are observed with an anoscope, proctoscope or sigmoidoscope to check for internal hemorrhoids. The doctor may recommend a barium enema only if he suspects colorectal cancer. Otherwise, imaging is not routinely done for hemorrhoids. In certain instances, a stool guaiac test or guaiac fecal occult blood test (gFOBT) may be ordered to detect blood in the stool that is not visible to the naked eye.
The doctor should know about any medications that the patient may be taking. Some medicines that may need to be stopped several days before the surgery include the following:
- Ibuprofen
- Aspirin
- Naproxen
- Warfarin
- Apixaban
- Rivaroxaban
- Clopidogrel
The patient is advised to stop smoking for two weeks prior to surgery as smoking can impede the healing process.
Routine blood and urine tests are carried out to determine the health status of the patient and rule out any underlying disease.
A chest x-ray and electrocardiogram (ECG) will be performed to rule out any heart or lung disease.
The patient is evaluated before surgery by the cardiologist and anesthetist and proclaimed fit for surgery.
The patient is instructed to get admitted to the hospital on the evening prior to the operation for undergoing certain procedures and for medications.
The patient will be asked not to eat or drink 6 to 12 hours prior to the surgery. These instructions should be strictly adhered to.
Saline enemas are also given on the morning of surgery to wash and cleanse the rectum and lower part of the large intestine of any fecal matter. This will enable the surgeon to get a clear view of the operating area.
The patient is advised to take a bath as usual and given a sterile surgical gown to wear before being taken to the theater.
What Happens During the Hemorrhoidectomy Procedure?
The surgical hemorrhoidectomy is performed in an operation theater. Any of the three types of anesthesia may be administered. Local anesthesia may be used around the anorectal area, producing a local effect. A spinal block involves administration of anesthesia in the vertebral column at the back, which anesthetizes the entire lower portion of the body. If general anesthesia (GA) is used, the patient will be unconscious and will not be aware of the operation at all.
During surgery, incisions are made around the hemorrhoid with a scalpel, cautery pencil (heat-generating electrical instrument) or laser. The swollen veins in the hemorrhoid are tied to prevent bleeding. The surgical wound can be left open or sutured. A medicated gauze is applied on the wound.
The following types of hemorrhoidectomies are performed:
- Rubber Band Ligation
- Injection Sclerotherapy
- Coagulation
- Stapled Hemorrhoidopexy (Procedure for Prolapse and Hemorrhoids – PPH)
- Conventional Surgical Hemorrhoidectomy
- Hemorrhoidal Artery Ligation Operation (HALO)
- New Techniques
Minimally Invasive Procedures: Rubber Band Ligation is a minimally-invasive procedure in which a rubber-band is placed around the base of the hemorrhoid. This cuts-off the blood supply and the hemorrhoid degenerates within a few days. This procedure is suitable for small internal hemorrhoid. Other procedures that are minimally invasive include sclerotherapy where a chemical solution such as 5% phenol almond oil is injected into the hemorrhoid to shrink it. It is relatively painless but not as effective as rubber band ligation. Coagulation treatment involves use of laser, infra-red rays or heat to harden and cause shrinkage of the hemorrhoid. The rate of recurrence may be higher in this procedure.
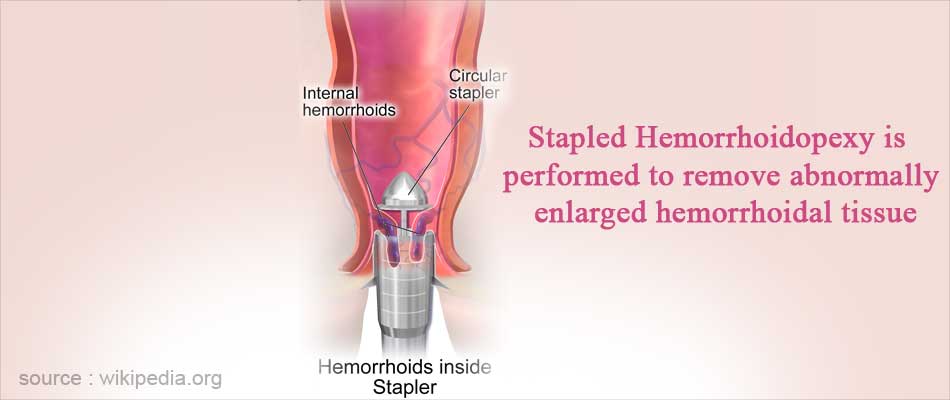
Stapled Hemorrhoidopexy: This procedure, also known as Procedure for Prolapse and Hemorrhoids (PPH), utilizes a circular stapling device that cuts away the excess hemorrhoidal blood vessels and staples-up the tissue. Stapled hemorrhoidopexy is associated with less post-operative pain and disability than conventional hemorrhoidectomy.
Conventional Surgical Hemorrhoidectomy: In this procedure an incision is made using a scalpel, electrocautery or laser. The hemorrhoidal mass is clamped, tied-up and then excised. The wound can be sutured and closed-up (closed hemorrhoidectomy) or left open (open hemorrhoidectomy).
Hemorrhoidal Artery Ligation Operation (HALO): This procedure is effective in case of larger hemorrhoids and where simpler procedures have failed. An ultrasound probe is used to locate the hemorrhoidal blood vessels, which are sutured to stop the blood supply to the hemorrhoid. This procedure is usually done along with Recto-Anal Repair (RAR), hence it is also termed as HALO-RAR.
New Techniques: The newer techniques involve modern strategies to remove the hemorrhoidal tissues. Harmonic scalpel excision is one such method where ultrasound waves are used to cut and seal blood vessels leading to and from the hemorrhoidal mass. This technique is used for large hemorrhoids and where bloodless surgery is required. A laser can be used to cut through the tissues with simultaneous cauterization, thereby sealing off any blood vessels. Atomization is one of the latest techniques where a vacuum is used along with an atomizer that breaks down and sucks-up the hemorrhoidal tissue mass.
What Happens after the Hemorrhoidectomy?
After the hemorrhoidectomy procedure is completed, the patient is transferred to the recovery room.
Recovery period can be short if local anesthesia is used, while substantially longer if GA is used. Spinal anesthesia usually takes a few hours to wear off. The patient lies on the back horizontally for at least an hour following surgery to prevent anesthesia induced headache, which can be intense and take a long time to subside.
The intravenous channel remains connected until the patient can take clear fluids by mouth as well as tolerate it. Since GA can cause nausea, oral intake of fluids can be delayed.
Once the patient can tolerate oral fluids, the diet can be changed to solid food.
Before discharge, the patient must regain full sensation of the lower part of the body. Moreover, the ability to urinate without catheter support is also a prerequisite for discharge.
What are the Risks & Complications of Hemorrhoidectomy?
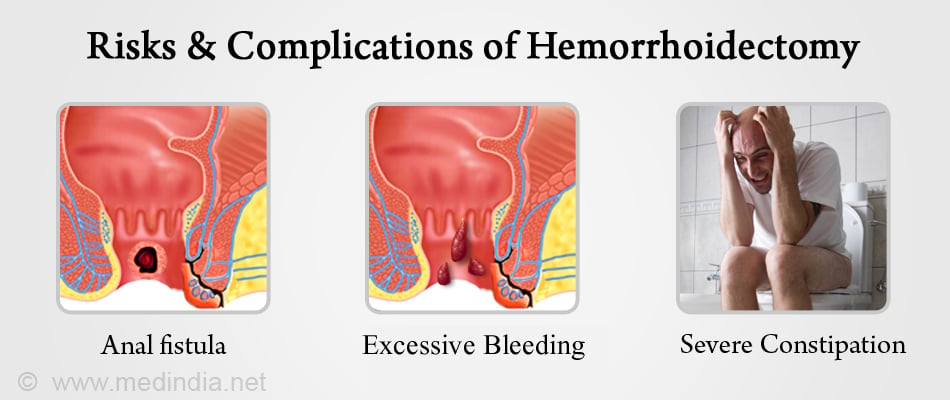
Hemorrhoidectomies have a high success rate. Most patients have a satisfactory recovery following surgery, without any complications or recurrence. However, even after a successful surgery, there is a 5% chance of recurrence. Complications are usually rare with hemorrhoidectomy, but nevertheless, can occur. One of the most painful complications of internal or external hemorrhoids is thrombosis. Other complications may include the following:
- Anal fistula or fissure
- Severe constipation
- Excessive bleeding
- Excessive fluid discharge from the rectum
- Fever of 38°C or higher
- Inability to urinate or have bowel movements
- Intense pain if bowel movements occur
- Redness and swelling in the rectal area
- Stenosis (narrowing) of the anus
- Recurrence of the hemorrhoid
Recovery after Hemorrhoidectomy
Patients can experience pain and discomfort during the first week following surgery, for which painkillers are usually prescribed.
An antibiotic such as metronidazole may be prescribed to prevent infections.
Minor to moderate bleeding can occur during defecation for the first two weeks following surgery. This is normal and usually subsides once the rectum has healed properly. If a pack was inserted in the rectum after surgery, it can be removed within a day after discharge.
An ice pack may be used for reducing the swelling and pain in the anal region. A mild anesthetic ointment can be applied before and after bowel movements to relieve the pain. Sitting upright is usually a major problem following surgery.
For maintaining a comfortable sitting posture, a special type of doughnut shaped cushion may be used. Soaking in a warm sitz bath can be comforting and relaxing, and can provide relief from pain and muscle spasms.
Avoiding constipation is crucial during convalescence. The doctor usually prescribes stool softeners and laxatives to prevent constipation.
The patients are advised not to lift heavy weights during the recovery period. Complete recovery occurs between 6 weeks to 2 months. However, the patient can generally resume work within 2 weeks.
Diet after Hemorrhoidectomy
For the first few days following hemorrhoidectomy, fluids are recommended along with a bland diet. This can include plain rice with lentils, bread, bananas, juices etc. Afterwards, the amount of roughage in the form of dietary fibers can be gradually increased. It is very important that after hemorrhoidectomy, the diet should contain high amounts of dietary fiber regularly. More fruits, vegetables and whole grains should be consumed. This will soften the stool and add bulk, thereby prevent straining during bowel movements. Thus, constipation, bleeding and increased chances of recurrence can be avoided. However, dietary fibers should be added gradually in order to prevent problems with gas build-up.

Health Tips
- Eat high fiber food after surgery: A diet high on fiber will ensure that the stool is soft and there is no straining or constipation during bowel movements.
- Soak in a sitz bath: Soak the anal area in a sitz bath 2 to 3 times a day to alleviate pain and swelling. The sitz bath can fit on the toilet seat, making it convenient to use.
- Maintain anal hygiene: Keep your anal area clean by washing regularly with warm water.
- Use topical ointments if required: You could go for an over-the-counter hemorrhoid cream for topically applying to the anal region. These creams can contain a local anesthetic or a steroid.
- Take oral pain killers as required: Your doctor may recommend oral pain killers like paracetamol, aspirin or non-steroidal anti-inflammatory drugs like ibuprofen to ease the pain and inflammation.