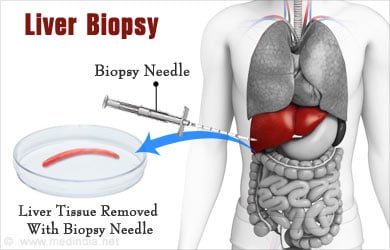
What is a Liver Biopsy?
A liver biopsy is the collection of liver tissue for the purpose of diagnosing liver disease. This procedure is increasingly common in India due to the high rates of fatty liver disease and chronic viral hepatitis (in some Indian states, the incidence of viral hepatitis infection is 2-12 times higher than in the United States.
Liver Biopsy can be done by:
- Per-cutaneously through the skin – A needle biopsy can be performed per-cutaneously through the skin into the liver using imaging guidance like ultrasound or CT scan under local anesthesia.
- Trans-venously - Accessing liver tissue through veins in the liver via the jugular vein.
- Laproscopic Biopsy - A surgical biopsy can be performed also laparoscopically.
- Open Surgical Biopsy - During an open surgical procedure. Surgical biopsies can be obtained using a needle (“core” biopsy) or a larger piece (“wedge” biopsy) can be removed.
How is a Liver Biopsy Done?
A liver biopsy procedure can be performed at the patient’s bedside, in the clinic or in the interventional radiology suite under ultrasound or CT guidance. Generally, two to three passes of the biopsy needle are necessary to provide sufficient tissue for the pathologist. Percutaneous biopsy is performed with local anesthetic and sometimes consious sedation. Rarely, general anesthesia is required (for example, infants or young children). A 4-6 hour period of close observation is required after biopsy to ensure the absence of complications. The procedure is usually performed on an outpatient basis.
A surgical biopsy is performed in the operating theater by a surgeon either laparoscopically or as part of an open surgical procedure. The patient is placed under general anesthesia by the anesthesiologist and a temporary breathing tube is inserted for mechanical ventialation while the patient is asleep. A laparoscopic biopsy involves very small incisions, so the recovery time is rapid.
Discharge from Hospital
Patients are usually discharged from the hospital after a 24 hour period of observation and they are back to their regular level of activity within a few days. If an open procedure is required, the recovery time will be longer because of the larger incision. Surgical “wedge” biopsies are preferred over needle biopsies because they provide more tissue for pathological diagnosis.

Processing of Liver Biopsy Specimen
The biopsy specimen is processed by the pathologist in order to view it microscopically. Overall changes in the normal liver architecture and evidence of inflammation can be seen with normal processing. Special stains can also be employed to diagnose specific illnesses. The pathologists, surgeons and hepatologists review the biopsy results together and decide upon appropriate treatment or additional diagnostic procedures.
Why are Liver Biopsies Performed?
The two most common reasons for liver biopsy are to diagnose a mass or tumor seen on imaging studies and to gauge the severity of tissue injury in diseases such as Hepatitis C Virus infection. Another indication is in diagnosing rejection or infection in patients who have had liver transplants.
Imaging studies such as ultrasound, CT scan and MRI can detect abnormal masses in the liver and both CT and MRI can definitively diagnose liver cancer (hepatocellular carcinoma) if certain criteria are met. If the diagnosis is unclear on imaging studies, that is, if there is a doubt if the mass appears benign or malignant, then biopsy should be performed to confirm the diagnosis and to direct appropriate therapy. Biopsy should not routinely be performed on liver masses that meet definitive imaging characteristics for cancer (e.g. arterial enhancement and venous “wash out” of the lesion on dynamic imaging and the presence of underlying liver disease such as cirrhosis) because the risks involved—although small—outweigh the benefit of any additional information from biopsy tissue.
Serial Biopsies of the Liver Pathology
Patients with chronic liver diseases such as Hepatitis B or C infection, fatty liver disease leading to non alcoholic steatohepatitis (NASH), or any number of other diseases leading to progressive fibrosis and ultimate cirrhosis, can be monitored by serial liver biopsies. Serial biopsies are especially important in determining response to treatments such as antiviral medications.
Liver transplant patients often undergo biopsies to detect rejection or infection. In certain cases, “protocol” serial biopsies are performed to detect recurrent disease (such as the case with transplant for Hepatitis C, which has a significant recurrence rate). Otherwise, biopsies are only performed if there are laboratory tests (liver function tests) or physical symptoms suggestive of rejection.
What are the Risks of Liver Biopsy?
Bleeding is the major complication - The risk of bleeding after biopsy is low (<1%) and depends on the extent of the patient’s underlying liver disease. In patients with advanced liver disease (cirrhosis and portal hypertension), this risk of bleeding increases because the diseased liver is not making blood clotting factors properly and portal hypertension causes a low platelet count (platelets are the cells responsible for initially forming blood clots) due to an enlarged spleen, or “splenomegaly”. The risk of mortality of liver biopsy is estimated to be between 0.01% and 0.1%.
Other potential complications that are less common include:
- Injury to adjacent structuressuch as the bowel, lung or gallbladder,
- Pain at the biopsy site,
- Infection
- Biopsy needle tract “seeding” of tumor cells during biopsy of malignant lesions.
Making Liver Biopsy Safe
Ultrasound or other imaging guidance during biopsy and careful post-procedure monitoring (frequent measurements of vital signs such as pulse and blood presuure, serial physical exams and post-biopsy labs to rule out bleeding) greatly minimize the risks involved. Also, the biopsy approach (percutaneous, transvenous or surgical) is determined by the degree of patient illness, with transvenous biopsy being reserved for the highest risk patients.






