What are the Complications of Liver Transplantation?
Given the complexity of liver transplantation, it is surprising that complication rates are so low and overall success is so high. The one year survival is 85-90% and at five years it is 70%. Death during the procedure is a rare event, occurring less than 1% of the time.
Infections: The most common cause of death after a liver transplant is infection, either a hospital acquired sepsis or an opportunistic infection resulting from the necessity of immunosuppressive drug use. Patients with liver failure tend to be naturally immunosuppressed, mostly as a result of malnutrition, so it is important not to give anti-rejection medicines in too high doses. Simple urinary tract infections or pneumonias can rapidly transform into life threatening infections in the liver transplant recipient.

Bleeding: Bleeding is not uncommon in liver transplantation because the liver is a very vascular organ and when the liver is not functioning properly, the blood becomes thin. Surgical bleeding is almost always a controllable situation, even if it means returning the patient to the Operation Theater to correct after the initial transplant. The newly transplanted liver usually starts synthesizing appropriate amounts of coagulation factors within minutes to hours, so postoperative bleeding is often surgical in nature.
Biliary leak or Strictures: Biliary leak or strictures occur 30% of the time with Living Donor Liver Transplant (LDLT) and 15% of the time with Deceased Donor Transplant (DDLT). Often, biliary complications can be managed non-surgically with the assistance of Hepatologists using endoscopy or Interventional Radiologists using catheter based approaches. Chronic biliary strictures can cause significant long term morbidity, including bile duct infections (cholangitis) and liver abscesses.
Primary Non Function of the Transplanted Liver: Primary Non Function, when the newly transplanted liver does not work at all, is fortunately a rare event (<1%) but requires immediate re-transplant to save the patient. Another complication that may require immediate re-transplant is hepatic artery thrombosis (“HAT”).
Hepatic Artery Thrombosis (HAT): occurs in 2-5% of cases and is more common when smaller vessels are being anastomosed (such as with Living Donor Liver Transplant or in pediatric liver transplant). Even if re-transplant is not required, there is significant morbidity associated with long term HAT, including repeated infections of the bile ducts and liver.
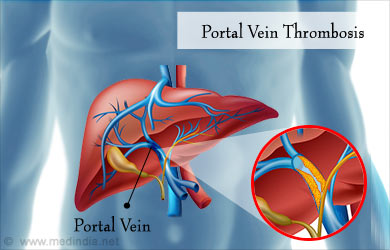
Venous Complications - of liver transplant include portal vein thrombosis and hepatic venous outflow obstruction. If portal vein thrombosis occurs early after transplant, it must be recognized and treated quickly, usually surgically but sometimes with catheter infusion based treatments by the Interventional Radiologists. Chronic portal vein thrombosis is usually well tolerated but can make re-transplant (if ever required) difficult to impossible. Hepatic venous outflow obstruction occurs when the veins draining blood from the liver into the inferior vena cava are too narrow (usually as a result of surgery), leading to congestion of the liver. If severe and longstanding, this can lead to ascites and renal failure.
Incisional Hernia: is quite common after liver transplant because patients with chronic liver failure often have very weak connective tissue as a result of malnutrition. The weak section of the abdomen leads to protrusion of the abdominal contents in the hernia. Incisional hernia rarely causes life threatening complications such as trapped (or “incarcerated”) bowel contents, but chronic discomfort can be easily alleviated with a simple hernia repair surgery.
Medical Complications
Rejection – when the grafted liver gets rejected by the body and this requires treatment. Usually it requires a biopsy to ascertain that there is rejection,
Opportunistic Infections – an immunosuppressed patient is prone to infections and this can result in infections by bacteria or viruses that normally cause no problems to a person.
Hospital acquired Vascular Complications: Like Deep Venous Thrombosis or pulmonary embolism.
Cardiac complications – like myocardial infarction
Neurologic complications – like stroke or due to adverse drug reaction
A fine balance of immunosuppression must be maintained: too little and the liver will reject, too much and the patient can easily suffer a life threatening infection.
Opportunistic infections are rarer in the current era of transplantation due to excellent prophylaxis regimens, sensitive surveillance tests and effective treatments for diagnosed infections. Other medical complications occur at similar rates as other major surgery patients, but they are poorly tolerated. Attention to detail and vigilance are paramount in the postoperative care of the liver transplant patient.






