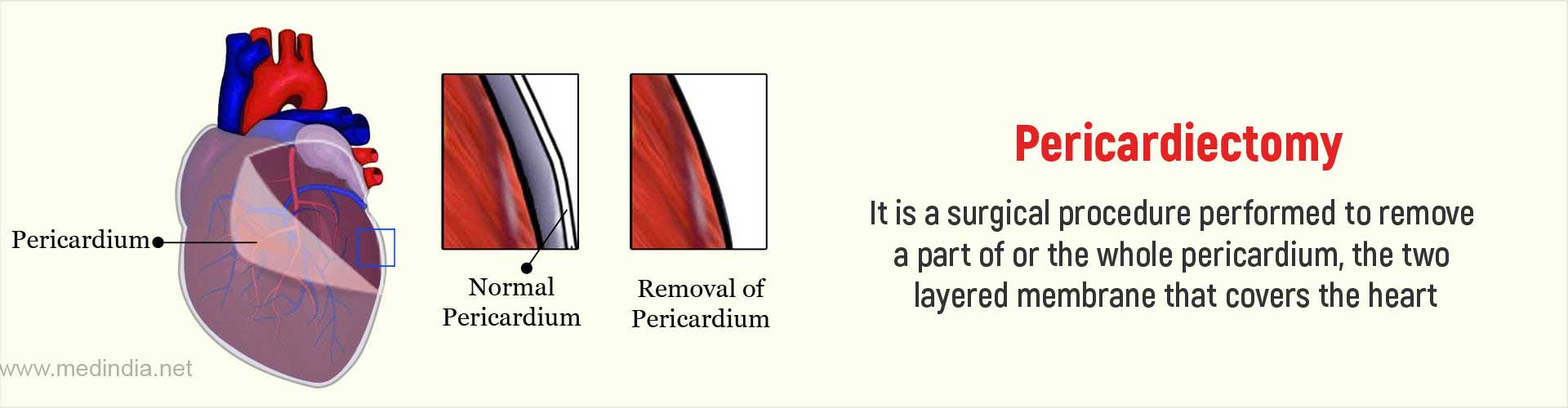
What is Pericardiectomy?
Pericardiectomy is a surgical procedure that is performed to remove a portion of or the entire pericardium. The pericardium is a two layered membrane that surrounds the heart. It is also referred to as pericardial stripping.
The 2 layers of the pericardium are the deeper visceral pericardium closely applied to the surface of the heart and the parietal pericardium which is the superficial layer. Between the two layers is the pericardia cavity, which contains a small amount of fluid that cushions the heart during its pumping function.
The pericardium is important because it avoids undue expansion of the heart when blood volume increases due to various disease conditions.
What are the Indications for Pericardiectomy?
The most common indication for pericardiectomy is chronic constrictive pericarditis. Recurrent attacks of inflammation of the pericardium result in it becoming thickened and scarred and calcified. The fibrosed and hard pericardium compresses the heart and restricts its movement.
Sometimes inflammation can also cause build-up of fluid within the pericardial cavity referred to as pericardial effusion. This fluid can also interfere with normal heart function and if the effusion does not respond to less invasive conservative measures and recurrent effusion occurs, surgery may be required.
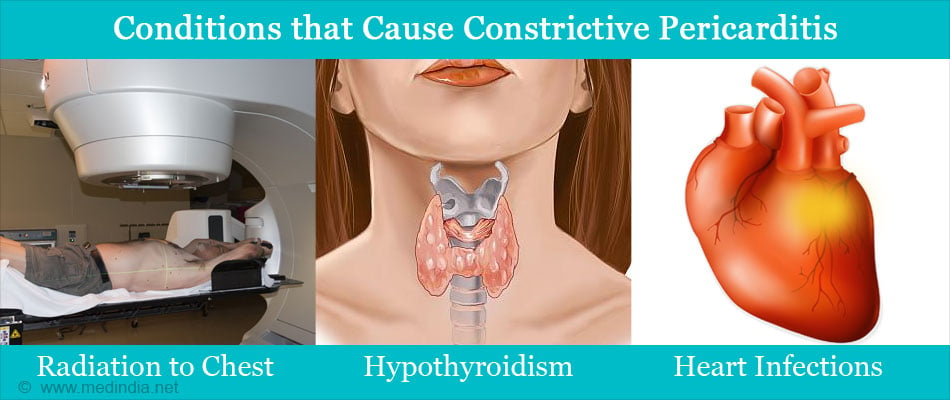
Conditions that cause constrictive pericarditis include the following:
- Infection of the heart or pericardium due to bacteria or viruses
- Primary cancers such as mesothelioma
- Cancer metastasis from elsewhere in the body
- Radiation to chest
- Autoimmune disease
- Reaction to certain medications such as Cyclophosphamide and Doxorubicin
- Hypothyroidism
- Complication of previous cardiac surgery
- Idiopathic (no identifiable cause)
How do you Prepare Before Pericardiectomy?
Once the decision to perform a pericardiectomy is made, the doctor will give specific instructions to follow to ensure optimal outcome of the surgery.
Starting about a week prior to surgery
- You may be asked to stop smoking for a few days prior to the procedure to aid in better healing and recovery.
- If you are on blood thinners such as aspirin you will be required to stop these prior to surgery. Be sure to inform your doctor about any underlying medical conditions and all current medications you are on.
- Routine blood tests and urinalysis will be advised to evaluate your general health status.
- A chest x-ray and electrocardiogram (ECG) are also done to determine the heart and lung condition.
- Additional investigations including an echocardiogram, CT or MRI imaging of the heart or cardiac catheterization to measure chamber pressures may also be requested.
- You will then be evaluated by an anesthetist who will examine you and declare that you are fit to undergo surgery.
- The pericardiectomy procedure is performed under general anesthesia.
- You have to get admitted to the hospital on the evening before surgery so that specific instructions can be followed and specific medications can be given.
- You will have to fast for at least 10 hours before surgery and avoid eating anything during this period.
- A mild sedative or anxiolytic may be given to ensure a good stress free sleep.
Morning of surgery
- On the morning of the surgery, the skin over the site of operation (chest) will be shaved and cleaned with antiseptic solution.
- You can have a normal bath and wear the surgical gown provided to you.
- Just before the surgery, you will be transferred to the operation theater where you will be shifted onto an operating table.
What Happens During Pericardiectomy
- The procedure is performed under general anesthesia. The anesthetist will give some intravenous drugs to put the patient to sleep and to produce analgesia.
- A tube will then be inserted into the wind pipe to oxygenate the lungs and to maintain respiration during the procedure.
- Vital signs such as heart rate, blood pressure and respiration will be continuously monitored during the procedure.
- The pericardium is usually reached by making a long vertical incision passing through
- the sternum or breast bone in the front part of the chest (median sternotomy). The breast bone will then be separated to access the pericardium. Occasionally another type of incision called thoracotomy incision performed on the side of the chest can be used to access the pericardium.
- Once the pericardium is reached, the surgeon will remove or strip a part of or the entire pericardium. Any other interventions if appropriate may also be done.
- After this the ribs and the breastbone will be wired back in place and the soft tissue and skin incisions closed in separate layers and the skin wound covered with dressing.
What Happens after the Pericardiectomy Procedure?
In the hospital
- Immediately after the procedure, you will feel a bit groggy and confused.
- A drainage tube might be placed into the side of the chest to drain the fluid in the chest. It is collected in a bag attached at its end and the fluid sent for lab analysis.
- You will be transferred to the post-operative room and kept under observation for a few hours while your vital signs are frequently monitored.
- Once the vital signs are stable you will be shifted to your room to allow recovery.
- Pain killers will be given for relief of pain and intravenous fluids given to maintain hydration.
- You may be allowed to take liquid food on the day following surgery and regular diet as soon as you are able to tolerate it.
- It may be necessary to remain in hospital for a few days. Prophylactic medications to prevent deep vein thrombosis will be given as long as you remain immobile.
- The drainage tube will be removed once the drainage of fluid stops.
- As soon as the doctor determines that you are fit to be discharged you will be sent home with instructions to follow.
Recovery at home
- You might be given pain killers to take orally as needed and vitamin supplements to aid speedy recovery.
- Advice on medicines, diet, exercising and permitted activities have to be strictly followed.
- Normal activities can be resumed within a week but lifting weights must be avoided.
- Consult your doctor immediately if there is fever, pain, excessive oozing or bleeding from the operative site.
- You will be given a followup appointment within a week to check your recovery and to remove the stitches.
What are the Complications of Pericardiectomy?
As with any surgery, pericardiectomy carries some risks. The risks depend on your age, general health condition and the seriousness of your underlying condition.
- Excess bleeding
- Infection
- Complications from anesthesia
- Abnormal heart beats or arrhythmias which can cause death in rare instances
- Pleural effusion or fluid buildup around the lungs
- Heart attack
- Low cardiac output syndrome
- Pneumonia
- Blood clot, which can lead to stroke or other problems
- Death
What is the Prognosis (Outlook) of a Pericardiectomy?
The outcome is generally better in younger patients who are healthier and have no major comorbidities compared to older patients with underlying medical conditions.
Studies have shown that the highest longterm survival was in patients who had idiopathic constrictive pericarditis followed by previous surgery and radiotherapy.