What is Radical Prostatectomy?
Radical prostatectomy is a surgical procedure where the entire prostate is removed along with the seminal vesicles and sometimes, with the nearby lymph nodes.
It is used in the treatment of prostate cancer that is limited to the gland and has not spread to the surrounding tissues or other parts of the body.

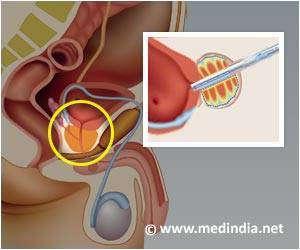
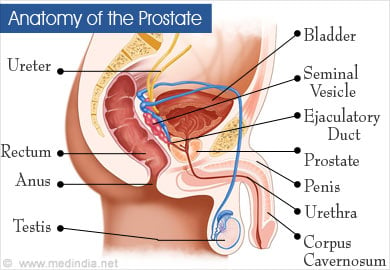
Anatomy of the Prostate
The prostate is a small walnut-sized gland that forms a part of the male reproductive system. It is located just below the urinary bladder, behind the pubic symphysis and in front of the rectum. It surrounds the upper part of the urethra, referred to as prostatic urethra. Fluid produced by the prostate passes into the urethra and forms a major part of the semen produced by men.
The prostate is surrounded by a covering called the prostatic capsule. Two small glands called the seminal vesicles are located behind the prostate on its upper aspect on either side. They also produce fluid that adds to the semen. The external urethral sphincter surrounds the urethra at the lower end of the prostate.
The dorsal venous plexus or Santorini plexus is located in the front of the prostate. Neurovascular bundles are located behind the gland on either side. These play an important role in erection of the penis. It is therefore important for the surgeon to know the anatomy of these structures in detail and protect them whenever possible during prostate surgery.
What is Localized and Advanced Prostate Cancer and their Treatment?
Localised prostate cancer is either a stage I or stage II disease and the cancer is confined within the capsule of the prostate gland. The treatment of choice of either a radical prostatectomy or radiotherapy to the gland depending on the age of the patient their performance status and associated diseases. The intent of treatment in such cancer is eradication of the cancer and to aim towards a complete cure. Radical prostatectomy is suitable for a relatively younger patient whose life expectancy is more than 10 years. Whereas radiotherapy is more suitable for older patients who has associated co-morbid factors.
Radical prostatectomy is performed on individuals diagnosed with prostate cancer that is localized to the gland. However, not every person is a candidate for the surgery. Very old patients may not be able to tolerate the surgery, and may benefit more with a wait-and-watch approach. Therefore, the requirement for the surgery is established on an individual basis.
Benefits of the procedure and the risks for urinary incontinence and erection problems should be clearly explained to the patient before the surgery, along with the necessity for the procedure.
In advanced prostate cancer, the cancer goes beyond the prostate capsule or it has spread to the lymph nodes. It is a stage III or IV disease. A complete cure may not be possible in these stage of the disease. The treatment of choice is more palliative and to control the cancer. The treatment is more hormonal to control the testosterone through chemical or surgical orchidectomy. But as time passes the tumor may get resistant and the patient may require chemotherapy.
What are the Types of Radical Prostatectomy?
Radical prostatectomy can be done either as an open surgical procedure or with the help of a laparoscope or a robot
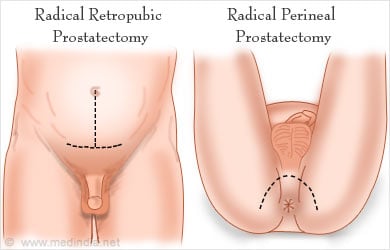
Types of open prostate surgery include the following:
- Radical retropubic prostatectomy, where the incision is made in the lower abdominal wall
- Radical perineal prostatectomy, where the incision is made in the region between the scrotum and the anus. A separate incision may be made on the lower abdomen to remove lymph nodes.
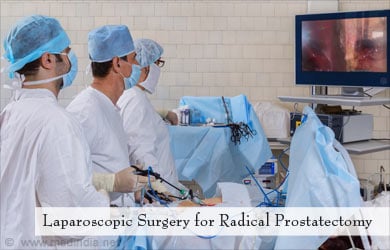
Laparoscopic or keyhole surgery is done through a few small incision. A laparoscope which enables visualization of the abdominal structures is introduced through one of the incisions. The images obtained are visualized on a screen. Surgical instruments are introduced through small holes to carry out the surgery. Laparoscopic surgery has several advantages over open surgery and includes:
- Reduced blood loss,
- Smaller skin scars,
- Less pain
- Early post- operative recovery
- and Early healing.
Types of laparoscopic surgery used for radical prostatectomy include:
- Robotic-assisted laparoscopic radical prostatectomy using da Vinci robotic interface. The actual surgery is done by three robotic arms, whose movements are controlled by a surgeon at a console. Robotic surgeries have the advantage of magnified 3D - visualization and better surgical precision, even in complex surgeries.
- Laparoscopic radical Prostatectomy
What are the Tests done before the Prostatectomy Surgery?
Tests done before a radical prostatectomy procedure include the following:
Prostate specific antigen (PSA) estimation: The blood levels of PSA are increased in prostate cancer. However, it is also raised in other conditions affecting the prostate like prostatitis, and therefore is not a reliable indicator of prostate cancer. Its level reduces within 6 weeks following prostate cancer surgery. If the levels do not reduce, residual cancer should be suspected. PSA is a good indicator in the follow up period of the cancer. Its rise indicates recurrence of the disease.
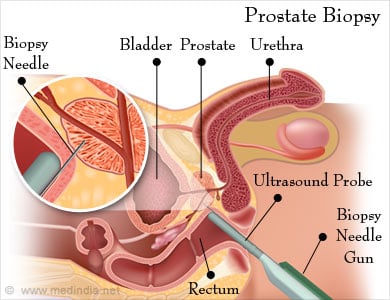
Prostate biopsy: Prostate biopsy is done under the guidance of trans-rectal ultrasound to visualise all areas of the prostate and used especially if the PSA is low (less than 20). If the PSA is very high (say over 100) it indicates a more diffuse disease and a trans-rectal probe may not be required for the biopsy as the whole gland clinically feels malignant.
To perform the biopsy the ultrasound probe is introduced through the anus towards the rectum, and the prostate is visualised on the screen of the ultrasound machine. A needle is then introduced through the rectum and multiple needle biopsies are taken from different areas of the prostate gland. Up to 12 different cores of tissues or sometimes even more are taken. These long filament like cores are transferred into formalin bottles and sent for examination. Each core has one bottle and there may be 12 or more bottles sent out for biopsy. More information about prostate biopsy is available at:
http://www.medindia.net/patients/patientinfo/biopsyprostate.htm
Biopsy of the seminal vesicles maybe required if there is infiltration of the gland.
CT scan / MRI: CT scan and MRI of the abdomen and pelvis confirm the presence of the cancer as well as indicate any spread to neighbouring structures.
For a CT scan, you will be asked to lie down still on a special table for a few minutes. A doughnut-shaped instrument will pass over the part to be screened, and images will be taken. A contrast may be injected into your vein; therefore you should inform the radiologist if you suffer from any allergies.
For an MRI, you will be placed inside a narrow tube, which can sometimes make you claustrophobic, if you have a fear of enclosed spaces. Few centres do offer more open MRI machines, but the drawback is that the pictures may not be as clear. The MRI machine makes loud clicking noises and it is advisable to ask for earplugs to help block these noises out.
Special MRI fusion biopsies have recently been advocated to getter yield of small cancer areas in the prostate gland.
Bone scan / Prosta-Scint scan: In these tests, a small amount of radioactive substance is injected into the blood, which gets localized in cancer cells in the bone in the case of bone scan, and in prostate cancer cells anywhere in the body in case of the ProstaScint scan. The radioactivity is detected with the help of a scanner. These tests thus detect if the cancer has spread to the bone or other parts of the body.
Other specialised imaging tests that may be used in the diagnosis of prostate cancer include contrast-enhanced color Doppler ultrasound, elastography to measure tissue elasticity, dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) and magnetic resonance spectroscopic imaging (MRSI). But all this is rarely required.
Routine tests: Routine tests which are done before any surgery include:
- Blood tests like hemoglobin levels, blood group, and liver and kidney function tests
- Urine tests
- ECG to study the electrical activity of the heart
- Chest x-ray
- In older group of patients, detailed assessment of the heart may be required to make sure that they are fit for surgery.
What is the Procedure for Radical Prostatectomy?
Whichever type of Radical Prostatectomy (open or laparoscopic or robotic) the general procedure is the same.
Type of Anesthesia - Radical prostatectomy is done under general anesthesia and sometimes under epidural anesthesia.
You will be asleep during the procedure and will not be aware of what is going on.
Pre-operative Check-up – Routine tests as indicated above are ordered a few days before the surgery. Admission is required a day or two before the surgery.
Day before Surgery -An enema is administered the previous afternoon or evening before the surgery along with gut sensitive antibiotics.
Fasting before surgery - Overnight fasting is required and occasionally intravenous fluid maybe required to keep you well hydrated. Sedation is sometimes required for good overnight sleep before the surgery.
Shift from the ward or room to the waiting area in the operating room - An hour or two before the surgery, you will be shifted to the operating room waiting area on a trolley.
Once the surgical room is ready, you will be shifted to the operating room.
Shift to the Operating room - The ambience in the operating room can sometimes be very daunting and a small amount of sedation can help overcome your anxiety. From the trolley, you will be shifted on to the operating table. As you look up, you will see the operating light console and at the head end will be the anesthesia machine. There may also be monitors to check oxygen levels, ECG and other vital parameters. A constant beeping sound may be present from the monitors, which may sometimes be irritating.
Anesthesia before surgery - The anesthetist will inject drugs through an intravenous line and make you inhale some gases through a mask that will put you in deep sleep for anesthesia. Once you are in deep sleep, a tube will be inserted into your mouth and windpipe to administer the anesthesia gases to overcome pain and keep you comfortable.
The Radical Prostatectomy Procedure – The radical prostatectomy surgery involves the following:
- The incision for the procedure depends on the type of surgery. During an open surgery, the incision is made either in the lower abdomen or the perineum, while laparoscopic surgery makes use of small multiple incisions.
- If lymph nodes have to be removed, they may be removed via a lower abdominal incision or through the laparoscopic method.
- As the tissues around the prostate are separated, care is taken to prevent bleeding from the dorsal venous plexus in front of the prostate.
- The prostate is separated from its surrounding tissue and ligaments.
- The neurovascular bundles are identified. Sometimes, neurovascular bundles on both sides are preserved, while in other cases the bundle on one side may have to be sacrificed. Preservation of neurovascular bundles may not be necessary in older men who already have problems with erection. Similarly, the bundles are not preserved if they are also affected by the cancer
- The seminal vesicles and vas deferens are also separated and removed
- The prostate is cut out along with its urethra, but without disturbing the external urethral sphincter. The cut ends of bladder neck and the urethra are stitched together.
- A drain is placed in the pelvic region to drain out any fluid that may accumulate. A catheter is passed through the urethra to drain urine from the bladder till healing of the surgical wound is complete.
The procedure can take 2 to 4 hours depending on the complexity of the procedure.
Waking up from Anesthesia – Once the surgery is over you will wake up and the tube down the wind pipe will be removed. You will be asked to open your eyes before the tube is removed. You will be sedated and the voice of the anesthetist may be faint. Once the tube is out, you may have cough and sometimes nausea.
There may be a tube going into the stomach called a nasogastric or Ryle’s tube to keep it empty. There will also be an intravenous line. You will remain on oxygen. Once fully awake, you will be shifted on the trolley and taken to the recovery room.
Recovery room – In the recovery room, a nurse will monitor your vitals and observe you for an hour or two before shifting you to the room or a ward.

Post-operative recovery – You will remain in the hospital for a few days following the procedure. Light foods may be allowed following the surgery.
Chest physiotherapy maybe started after 24 hours to prevent chest infection.
DVT Prophylaxis – Early movement of your legs and some mobilization prevents DVT or deep vein thrombosis, where a clot is formed in the deep veins of the legs. The clot can travel up to the lungs and even be fatal. Other measures like small dose of heparin and special stockings may also be used.
Painkillers may be prescribed depending on the extent of the pain.
Instructions following discharge – Your doctor will advise you to drink plenty of fluids and check the color of the urine in the catheter on a regular basis. The catheter may be removed 7 to 14 days after the surgery depending on your recovery. You will receive instructions regarding care for the catheter and urine bag.
Once the catheter is removed, you may have to wear incontinence pads for some time till you become fully continent, which may even take a few months. You will be taught Kegel exercises to strengthen your pelvic floor muscles. Pelvic floor muscles support your bladder and rectum. These exercises are very simple and involve the following steps:
First, identify the muscles that need exercise by trying to stop passing urine midway. Notice which muscles you have tightened. While doing the exercise, contract these same muscles and hold for a few seconds, and then relax over the next few seconds. You will have to repeat the exercise several times in the day as advised by your doctor.
Return of Sexual function: If your doctor has done a nerve sparing operation, your sexual function will return, but it will take a few months to even up to 2 years. Your doctor may prescribe tablets like Viagra for early recovery of erectile function.
Follow-ups: You will have to make repeated trips to the hospital for follow-ups. You may need hormonal or radiotherapy to prevent recurrence of the condition. PSA levels should be measured on a regular basis to check for recurrence of cancer.
What are the Complications of Radical Prostatectomy?
Complications of radical prostatectomy include the following:
- Impotence. The incidence of erection problems or erectile dysfunction has decreased following neurovascular bundle preservation procedures.
- Narrowing of the outlet of the urine from the bladder due to scarring. This condition is called bladder neck contracture
- Excessive blood loss and injury to surrounding structures like rectum. These complications are less common with robotic surgery
- Urinary incontinence if the urinary sphincter is damaged
- Infections, if adequate aseptic precautions are not taken during surgery
- Hernia, where outpouching of abdominal tissue occurs through a weak spot in the abdomen