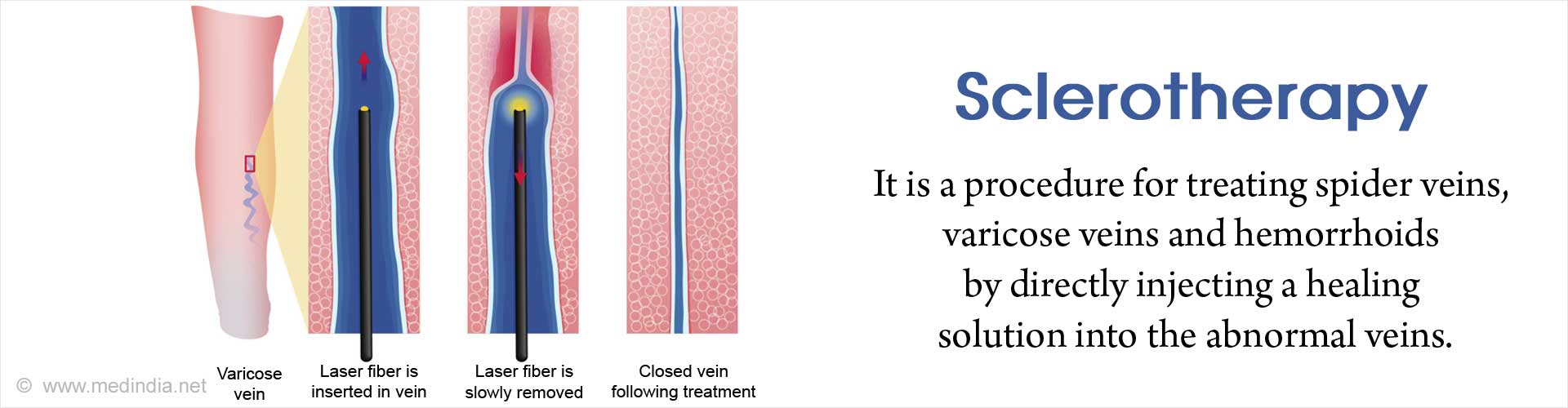
What is Sclerotherapy?
Sclerotherapy is a procedure used to treat spider veins, varicose veins and hemorrhoids in adults by directly injecting a solution called the sclerosant into the veins. In children it is used in the same manner to treat vascular and lymphatic malformations. It is the treatment of choice mainly for small varicose veins. Injecting the unwanted veins with a sclerosing solution or a sclerosant causes the target veins to immediately shrink, so that they can be naturally absorbed by the body once they dissolve. This can take from a few weeks to more than a month. Sometimes repeat sclerotherapy may be needed.
Sclerotherapy is considered generally safe although a few adverse effects have been reported.
What is the Mechanism of Action of Sclerosants?
Sclerotherapy is a non-invasive procedure that takes about 10 minutes to perform with a minimal downtime compared to an invasive varicose vein surgery.
The diluted sclerosant can be in the form of a liquid or foam and is injected multiple times into the abnormal surface veins of the affected leg. The agent irritates the lining of the vessels, makes them swell and stick together (thrombophlebitic reaction). This leads to the production of a fibrous cord and over time the veins shrink and form scar tissue that fade away. The blood is forced to reroute through normal veins. The dead veins are reabsorbed into local tissue.
After the procedure, the patient's leg is wound with either stockings or bandages so as to compress the veins. These bandages have to be worn usually for two weeks after treatment.
The latest developments in sclerotherapy use ultrasonographic guidance and foam sclerotherapy. The ultrasound helps to visualize the underlying vein in order to direct the physician to deliver and monitor the injection.
Foam sclerotherapy involves injecting “foamed sclerosant drugs” within a blood vessel using two syringes known originally as the Tessari method (3-way tap method), one containing the sclerosant and the other containing gas. The modified version known as the Whiteley-Patel modification uses 3 syringes to make long lasting foam. Small volumes of sodium tetradecyl sulfate or polidocanol are made into foam by rapidly mixing and agitating them with a small amount of air or a physiological gas (carbon dioxide) in a syringe or by using mechanical pumps to increase the surface area of the drug.
A map of all the varicose veins and real-time monitoring of the injections where the physicians can see the sclerosant entering the veins are done using ultrasound. This is done so that all the abnormal veins are treated. Ultrasound scans confirm closure of the treated veins, and to identify and treat residual veins.
What are the Advantages and Disadvantages of Ultrasound Guided Foam Sclerotherapy?
Foam sclerotherapy is a modification of conventional sclerotherapy procedure and suited to treat large varicose veins. It has several advantages over the conventional procedure.
- To treat all sizes of varicose veins including larger varicose veins like the great saphenous vein (GSV) and small saphenous vein(SSV) (superficial veins of the leg).
- In the foamed state, the drug is more efficacious than the liquid form.
- It causes better thickening of the vessel wall and sealing off the blood flow because it does not mix with the blood in the vessel.
- There is no dilution of the drug since it displaces the blood rather than mixing with it and thus causes maximal sclerosant action.
- Controls reflux from the sapheno-femoral and sapheno-popliteal junctions.
- Additionally closes the “feeder veins” that form the basis of the spider veins thereby cutting their source.
There are however, some disadvantages associated with foam sclerotherapy. These include:
- Redness and itching over the area
- Headaches
- Low back pain
- Formation of tiny clots or microembolisms
- Altered skin color over treated site
- Escape of foam from the veins into the heart and to the brain
What are some of the Sclerosants used in Sclerotherapy?
The sclerosants most commonly used worldwide are sodium tetradecyl sulphate (STS), and polidocanol and are available in different concentrations depending on the size of the vein being treated.
In general, the agents used in the injection can be classified into detergents, chemical irritants, and osmotic agents.

Detergents:
Mechanism of action - destroy vein cell membrane through protein denaturation
Examples - sodium morrhuate, ethanolamine oleate, sodium tetradecyl sulfate (STS), and polidocanol.
Chemical irritants:
Mechanism of action - damage the cell wall by direct caustic destruction of the epithelium
Examples - polyiodinated iodine and chromated glycerin
Osmotic agents:
Mechanism of action - damage the cell by shifting the water balance
Examples - hypertonic sodium chloride solution and sodium chloride solution with dextrose.
What are the Risks, Side Effects and Complications of Sclerotherapy?
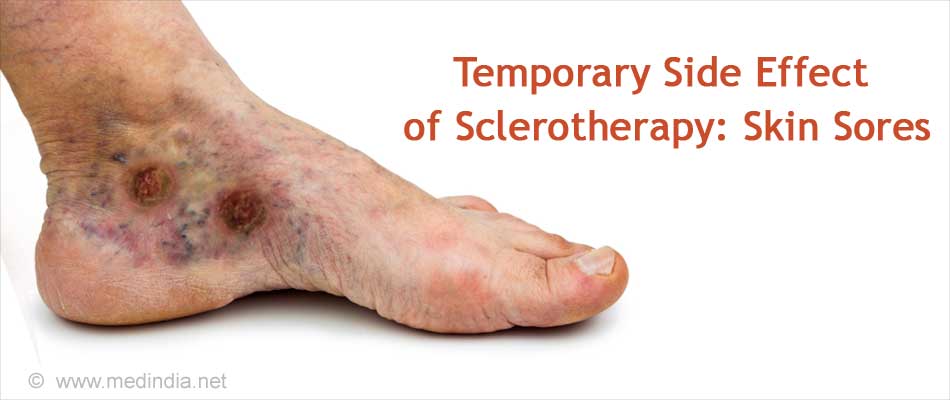
After a sclerotherapy procedure there can be temporary side effects present at the site of the injection that usually disappear within a few days or weeks. These include:
- Bruised red patches
- Skin sores
- Development of many tiny red blood vessels or telangiectatic matting that has to be treated with repeat sclerotherapy or laser
- Darkened lines or spots on the skin
- Sometimes, if the sclerosant is injected outside the vein skin tissue necrosis could occur that could take months to heal.
Less common but more serious complications might require some form of treatment include:
- Inflammation or swelling around the injection site that could cause discomfort. Aspirin helps reduce the inflammation.
- Visual disturbances, nausea and headaches if any air bubbles are present in the bloodstream after the procedure. These bubbles could travel to the heart, lung and brain.
- Blood clot or thrombosis may occur in the treated vein that might need to be drained. If the clot travels into a deeper vein it may cause deep vein thrombosis of the leg.
- Chest pain, dizziness or blood when you cough could mean a very rare complication of sclerotherapy where the clot formed in the legs moves from there to the lungs and could block a vital artery (pulmonary embolism ).
- So far there is one reported case of stroke after ultrasound-guided sclerotherapy due to an unusually large dose of sclerosant foam that was injected.
What are the Latest Developments in Treating Varicose Veins?
Radiofrequency ablation involves inserting a thin tube (catheter) into an enlarged vein, and heating the tip of the catheter using radiofrequency energy. As the catheter is pulled out, the heat destroys the vein; the vein collapses and seals shut. The catheter can also be heated with laser energy. Radiofrequency ablation is used to treat the great saphenous vein, the small saphenous vein, and the perforator veins (connecting veins that transport blood from the superficial veins to the deep veins).
ClariVein® occlusion catheter system is a relatively new minimally invasive approach that uses a combination of damage to the endothelial cells by mechanically agitating them and chemical injury to induce closure of the veins. It uses a liquid sclerosant infusion at the tip of the catheter. It is used for the great saphenous vein and the small saphenous vein.