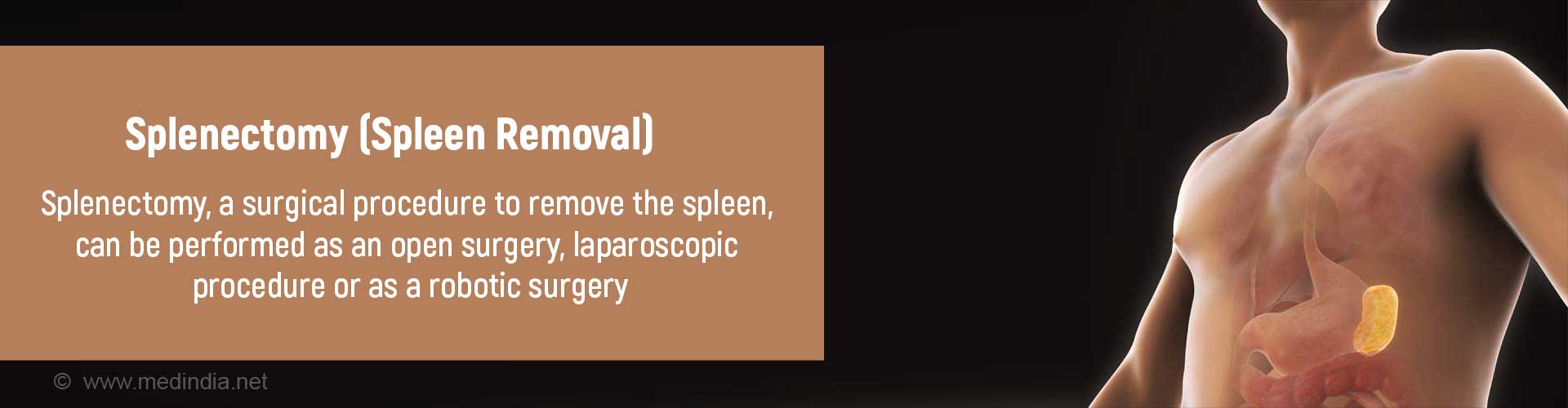
What is Splenectomy?
Splenectomy is a surgery done to remove the spleen for the treatment of various conditions. It can be performed as an open surgery through a large abdominal incision, or with the help of a telescopic instrument called a laparoscope, or through robotic surgery.
Anatomy of the Spleen
The spleen is a small organ located in the upper left abdomen behind the lower ribs and just below the diaphragm. Blood vessels and nerves supplying the spleen enter and exit the spleen via its hilum. The spleen is connected by connective tissue ligaments to the stomach and the left kidney.
Though the spleen may not be as well-known as its neighbors, the stomach, liver, left kidney and colon, it has important functions – it produces blood cells, helps to develop immunity to fight infections, and removes dead or damaged cells from the circulation.

What are all Types of Splenectomy?
Depending on the operative procedure adopted, splenectomy can be classified as:
- Open splenectomy. Open splenectomy is performed through a large incision in the upper abdomen.
- Laparoscopic splenectomy. Laparoscopic splenectomy is done through smaller incisions with the help of a telescopic instrument called a laparoscope. It is associated with lesser pain, faster wound healing, shorter hospital stay and better cosmetic results following the surgery.An open surgery is however preferred over a laparoscopic procedure for trauma cases and for splenic cancer(due to the risk of spreading the cancer). Very large spleens may present technical difficulties during removal.
- Robot-assisted splenectomy: Robot-assisted surgery is an alternative to laparoscopic surgery. It provides a three-dimensional view and better access to the surgical site. The cost of the procedure and its limited availability have hindered its widespread use.
Depending on the amount of spleen removed, the splenectomy may be partial or complete.
- Complete splenectomy is when the entire spleen is removed.
- Partial splenectomy is when where only a segment of the spleen is removed. The cut ends are brought together to seal the defect.
What are the Indications of Splenectomy?
Splenectomy may be performed for the following conditions:
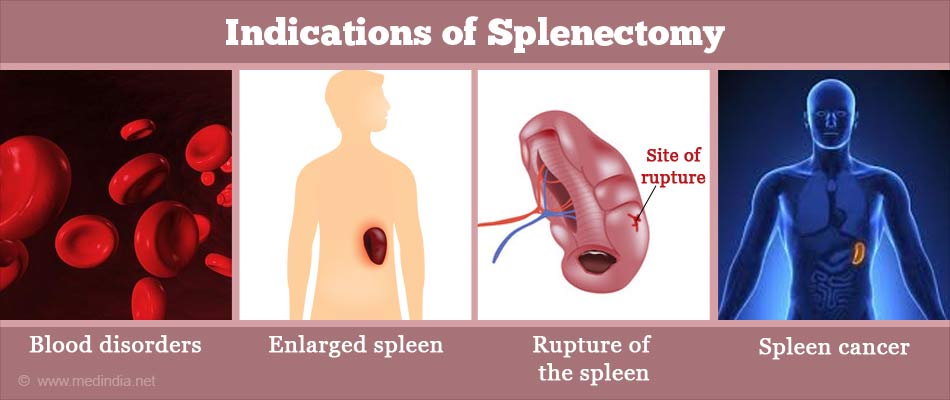
Blood disorders which may include:
- Idiopathic thrombocytopenic purpura (ITP) in patients who fail to respond to medical treatment. ITP is a condition where the body destroys its own platelets.
- Hereditary spherocytosis. In this genetic blood disorder, the red blood cells are larger than normal in size and break down when they pass through the tiny splenic blood vessels
Autoimmune hemolytic anemia - In this group of blood disorders, the body destroys the red blood cells faster than they are formed, resulting in anemia
- Other blood and bone marrow disorders like hairy-cell leukemia, chronic idiopathic myelofibrosis, and splenic lymphoma when indicated
Enlarged spleen, where the spleen sequestrates excess blood cells and destroys them. The spleen may be enlarged in the following conditions:
- Tropical splenomegaly due to infections like malaria, kala azar and schistosomiasis
- Felty’s syndrome, which is characterized by an enlarged spleen, low white blood count (neutropenia) and rheumatoid arthritis
- Idiopathic splenomegaly, where the cause of the enlarged spleen is not known
Rupture of the spleen, which may occur due to:
- Blunt trauma, for example, due to a blow on the spleen
- Penetrating trauma, for example, due to a knife piercing through the spleen
- Spontaneous rupture, which may occur in disease conditions like malaria and infectious mononucleosis
- Trauma during surgery on the neighboring organs
Patients with rupture of the spleen with low blood pressure require emergency surgery.
Splenic vein thrombosis, where the drainage of blood from the spleen is obstructed by a clot in the splenic vein
Aneurysm of the splenic artery. An aneurysm is a localized ballooning of an artery which can burst at any time resulting in instant death
Large cysts of the spleen, which may be due to:
- Parasitic infections
- Trauma
- Congenital (present at birth)
Cancers of the spleen, which include:
- Lymphoma, to stage the cancer
- Fibrosarcoma
- Angiosarcoma
Abscess of the spleen
It must however be remembered that splenectomy is not done for all patients with the above conditions, but is only done when it is really required and the benefit of removing it far outweighs the disadvantages of not having a spleen.
What happens before, during and after Splenectomy?
Before splenectomy, tests are done to confirm the need for the splenectomy. These include:
- Blood tests that include complete blood counts, a smear examination, bleeding and clotting tests.
- Bone marrow aspiration and biopsy examination, which may be done in certain cases like lymphoma.
- Endoscopy to check for dilated blood vessels (varices) in the upper digestive tract. The varices may be a sign of splenic vein thrombosis or portal hypertension and can bleed easily.
- Ultrasonography, which is an imaging test that can be done on an emergency or a routine basis to identify any pathology that could require splenectomy. It can determine the size of the spleen – a size of between 11 and 20 cm is classified as moderate enlargement while a size of more than 20 cm is considered as severe enlargement.
- CT (computerized tomography) scan with contrast, which provides more detailed information and can be used to study the blood vessels of the spleen, the presence of accessory spleens, and the presence of enlarged lymph nodes in suspected cancer.
Routine tests: Routine tests which are done before any surgery include:
- Blood tests like hemoglobin levels, blood group, and liver and kidney function tests to determine the patient’s health status
- Urine tests. Urine infection should be ruled out prior to the procedure
- Electrocardiogram (ECG) to study the electrical activity of the heart
- Chest x-ray
In older patients, a detailed assessment of the heart may be required to make sure that they are fit for surgery.
Type of Anesthesia: Splenectomy is done under general anesthesia. You will be asleep during the procedure and will not be aware of what is going on.

Pre-operative Check-up: Routine tests as indicated above are ordered a few days before the surgery. Since your immunity will be affected following the splenectomy, vaccination against pneumococcal, meningococcal and Hemophilus influenzae infections will be given 3 weeks prior to surgery. Medications like aspirin should be stopped around a week prior to the procedure. Admission is required a day before the surgery. Informed consent is obtained. These preparations can be skipped for individuals undergoing emergency splenectomy.
The Day before Surgery: An enema is administered the previous afternoon or evening before the surgery along with gut-sensitive antibiotics.
Fasting before Surgery: Overnight fasting is required and occasionally intravenous fluid maybe required to keep you well hydrated. Sedation is sometimes required for good overnight sleep before the surgery.
Shift from the Ward or Room to the Waiting area in the Operating room: An hour or two before the surgery, you will be shifted to the operating room waiting area on a trolley. Once the surgical room is ready, you will be shifted to the operating room.
Anesthesia before Surgery: In the operating room, the anesthetist will inject drugs through an intravenous line and make you inhale some gases through a mask that will put you in deep sleep.
During the procedure:
For the laparoscopic procedure, four to five small incisions will be made and ports will be introduced into the abdomen so that the laparoscope and the instruments can be introduced through them. Carbon dioxide will be insufflated to increase the visibility inside the abdomen.
The connective tissue attachments of the spleen to the neighboring organs in the abdomen will then be cut, along with coagulation or ligation of blood vessels that could cause bleeding.
The spleen that is freed from all its attachments will then be removed through a larger incision on the abdomen, or through a port with the help of a puncture-resistant bag. The spleen will be fragmented inside the bag before being brought out through one of the ports.
The abdomen will also be examined for any accessory spleens, which should be removed during the same sitting to prevent recurrence of the primary disorder for which the procedure was carried out.
If gallstones are also present, you will be turned on your back, and the gallbladder will be removed during the same surgery.
Once confirmed that there are no bleeding spots, the instruments will be removed, the abdomen deflated, the ports withdrawn, a drainage tube inserted, and the incisions will be closed with stitches. Platelet transfusion will be administered if necessary.
If the procedure cannot be completed through laparoscopy, it may be converted to open surgery.
For the open procedure, the surgeon will make a large incision on the abdomen and insert her/his hand along the convex surface of the spleen. The ligaments that attach the spleen to the surroundings will be cauterized or tied if they contain blood vessels and cut. The separated spleen will then be delivered through the wound. The abdomen will also be checked for accessory spleens or bleeding spots, and if all appears fine, it will be closed in layers.
Robotic surgery is similar to laparoscopic surgery. During robotic surgery, the surgeon will sit at a console and guide robotic arms to perform the surgery with utmost precision. The procedure, however, is not as widely available as laparoscopy, and requires an expensive set-up and surgeons trained in the procedure.
After the Procedure:
Waking up from General Anesthesia: Once the surgery is over you may wake up feeling a bit groggy due to anesthetic effect. Once fully awake, you will be shifted on the trolley and taken to the recovery room.
Recovery room: In the recovery room, a nurse will monitor your vitals and observe you for an hour or two before shifting you to the room or a ward.
Post-operative recovery: You will remain in the hospital for a few days following the procedure. You will receive intravenous fluids and will be allowed to take in liquids once your bowel sounds return. You will be slowly shifted to semi-solid foods and later to solid foods. Chest physiotherapy may be started after 24 hours to prevent chest infection. The abdominal drain will be removed once the drainage is minimal. Blood counts will be measured on the next day following the surgery. If you were taking steroids before the surgery, they will be reduced following the surgery. Antibiotics will be prescribed to prevent infection and pain relievers to reduce pain.
Early movement of your legs and some mobilization will be encouraged to prevent DVT or deep vein thrombosis, where a clot is formed in the deep veins of the legs. The clot can travel up to the lungs and even be fatal. Other measures like special stockings may also be used to prevent DVT.
Discharge from hospital: Once your wounds have healed and you can eat normal food, you will be discharged from the hospital. Restrict activities for six to eight weeks and follow up with your doctor on a regular basis as advised.
What are the Complications of Splenectomy?
Like any other surgical procedure, splenectomy is also associated with complications which may include the following:
- Postoperative pain
- Excessive internal bleeding, especially in cases of massive splenomegaly
- Injury to the pancreas with serious consequences
- Infection - wound infection, abscess formation, sepsis or pneumonia may occur. A particular infection to watch out following splenectomy is overwhelming post splenectomy infection (OPSI). OPSI is an overwhelming infection with meningococci, pneumococci, or H. influenzae. It is therefore necessary to vaccinate individuals before the surgery to prevent the infection
- Venous thromboembolism (clot in a vein) resulting in DVT (deep vein thrombosis), pulmonary embolism which may be fatal and thrombi in other veins,
- Collapse of the lungs
- Failure of the bowels to move following surgery (paralytic ileus)
- Splenosis - accidental transplantation of pieces of spleen in the abdomen. They could result in recurrence of the primary disorder.