- Keratoprosthesis - (https://webeye.ophth.uiowa.edu/eyeforum/tutorials/cornea-transplant-intro/6-kprosth.htm)
- Boston Type 1 Keratoprosthesis: Updated Perspectives - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7196770/)
- Boston type | keratoprosthesis versus penetrating keratoplasty following a single failed corneal graft - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9905503/)
- Boston type 1 keratoprosthesis from patient selection through postoperative management: a review for the keratoprosthetic surgeon - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4798197/)
About
Keratoprosthesis refers to both the implant itself and the surgical procedure used to implant the prosthesis.
Implant: Keratoprosthesis implant is a fake cornea placed in the eye to replace a damaged or sick cornea. Typically, manufacturers make this device using materials such as clear plastic polymethylmethacrylate (PMMA) or other biocompatible materials. The implant has a part for vision and a part for stability, sometimes with a tissue graft for integration.
Surgical Procedure: Keratoprosthesis surgery is the surgical procedure used to implant the artificial corneal device into the eye. The surgeon removes the damaged or diseased cornea and securely implants the keratoprosthesis into place during the surgery. The surgery uses careful techniques to place and integrate the device well, while reducing the chance of problems(1✔ ✔Trusted Source
Keratoprosthesis
Go to source).
Types of Keratoprosthesis
Different types of keratoprosthesis include:
- Boston Keratoprosthesis
- Boston Type I Keratoprosthesis: Comprising a clear plastic PMMA optic and back plate, often including a corneal graft, secured with a titanium locking ring. This type is typically used for severe corneal diseases or ocular surface disorders.
- Boston Type II Keratoprosthesis: Similar to Type I but with a longer optic extending through the upper eyelid opening. It is indicated for severe cicatrizing ocular surface diseases.
- Osteo-Odonto-Keratoprosthesis (OOKP): This involves using a tooth as a support structure for the optic. The tooth is modified and implanted to support the artificial corneal device. OOKP is indicated for severe corneal diseases with inadequate posterior corneal support.
- AlphaCor Keratoprosthesis: A synthetic corneal device made of biocompatible hydrogel material that allows for tissue integration. It is used for patients unsuitable for traditional corneal transplantation.
- Fyodorov-Zuev Keratoprosthesis: Developed in Russia, this type is designed for easy implantation and indicated for visual rehabilitation for patients with severe corneal conditions leading to corneal blindness(2✔ ✔Trusted Source
Boston Type 1 Keratoprosthesis: Updated Perspectives
Go to source).
Did You Know?
The Boston Type I Keratoprosthesis emerges as the most prevalent keratoprosthesis device utilized in the United States. Clear plastic and titanium make up its composition, and it securely holds a corneal graft in place.Keratoprosthesis Indications
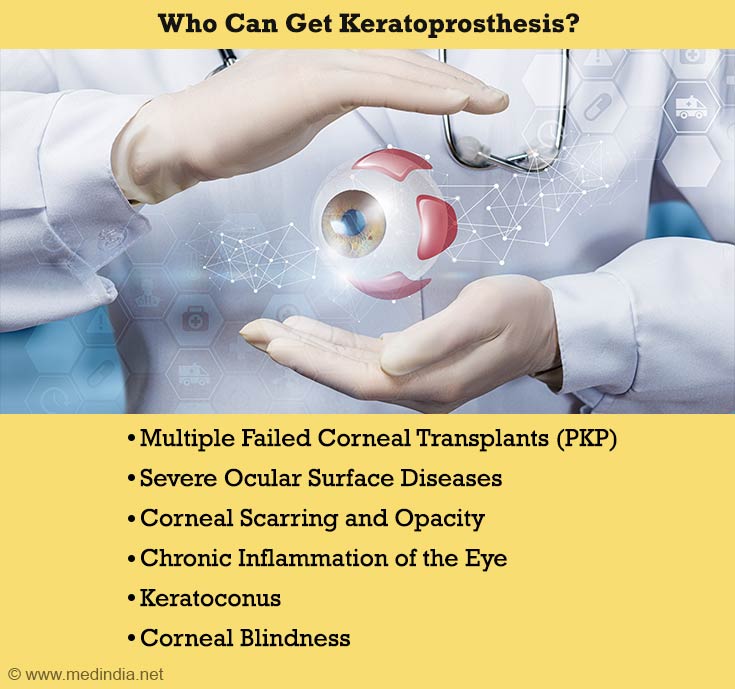
Some common indications for keratoprosthesis include:
Multiple Failed Corneal Transplants (PKP): Patients who have experienced repeated failure of penetrating keratoplasties (PKPs) due to conditions like corneal graft rejection or vascularization may be candidates for keratoprosthesis.
Severe Ocular Surface Diseases: Individuals with severe ocular surface disorders such as Stevens-Johnson syndrome, ocular cicatricial pemphigoid, aniridia, chemical injuries, and other conditions causing limbal stem cell deficiency may benefit from keratoprosthesis.
Corneal Scarring and Opacity: Patients with extensive corneal scarring or opacity that impairs vision and cannot be effectively treated with conventional corneal transplantation may be considered for keratoprosthesis.
Chronic Inflammation of the Eye: Conditions associated with chronic inflammation of the eye, such as autoimmune diseases like rheumatoid arthritis or scleritis, may necessitate keratoprosthesis in cases where inflammation compromises corneal integrity and function.
Keratoconus: In advanced cases of keratoconus where traditional treatments like contact lenses or corneal collagen cross-linking are insufficient to improve vision, keratoprosthesis may be considered as an alternative option.
Corneal Blindness: Patients with corneal blindness resulting from various etiologies, including trauma, infection, or congenital conditions, may undergo keratoprosthesis to restore vision and improve quality of life(3✔ ✔Trusted Source
Boston type | keratoprosthesis versus penetrating keratoplasty following a single failed corneal graft
Go to source).
Patient Selection and Management
Patient Selection
Patients with a history of multiple failed penetrating keratoplasties (PKs) often constitute primary candidates for keratoprosthesis transplantation. Keratoprosthesis may be helpful for people with severe eye conditions. These conditions include keratitis or ocular surface diseases caused by limbal stem cell failure. Examples of such conditions are Stevens-Johnson syndrome, ocular cicatricial pemphigoid, aniridia, or chemical injuries.
Keratoprosthesis Patient Management
Keratoprosthesis patient management involves pre-operative evaluation, surgical planning, post-operative care, and long-term follow-up to optimize visual outcomes, monitor for complications, and address ocular surface health.
Close collaboration between ophthalmologists, optometrists, and other healthcare providers is essential to ensure comprehensive and personalized care for keratoprosthesis patients(4✔ ✔Trusted Source
Boston type 1 keratoprosthesis from patient selection through postoperative management: a review for the keratoprosthetic surgeon
Go to source).
Keratoprosthesis Surgery
The keratoprosthesis implantation procedure follows a meticulous series of steps to ensure optimal outcomes for patients.
Pre-operative Preparation
Before the surgery, thorough pre-operative assessments ascertain patient suitability and enable tailored treatment plans. These assessments include evaluating corneal integrity, ocular health, and systemic factors impacting surgery.
Pre-operative Assessments:
- Corneal Topography and Pachymetry: Assess corneal shape and thickness.
- Ocular Surface Evaluation: Evaluate tear film quality, ocular surface integrity, and presence of inflammation.
- Systemic Evaluation: Assess patient's general health status and medication history.
Surgical Technique
- Partial-thickness Trephination:
- The process starts by making a small hole in the cornea to place the keratoprosthesis.
- Utilization of specialized trephination tools ensures accurate and uniform corneal incisions.
- Corneal Resection:
- The surgeon carefully removes the patient's cornea with curved scissors to make space for the keratoprosthesis.
- Careful dissection minimizes trauma to surrounding tissues and facilitates optimal wound healing.
- Keratoprosthesis Implantation:
- Implant is carefully placed and secured onto the host tissue using sutures for stability and integration.
- Selection of suture materials and techniques depends on patient-specific factors and surgeon preference(4✔ ✔Trusted Source
Boston type 1 keratoprosthesis from patient selection through postoperative management: a review for the keratoprosthetic surgeon
Go to source).
Patient Benefits from Keratoprosthesis
Improved Visual Acuity: Keratoprosthesis can significantly improve visual acuity, especially in patients with severe corneal diseases or conditions that cannot be adequately corrected with glasses or contact lenses.
Stabilization of Corneal Conditions: For patients with progressive corneal thinning or irregularities, keratoprosthesis can stabilize the cornea, preventing further deterioration of vision and potentially halting the progression of the underlying condition.
Reduced Dependence on Visual Aids: Many patients who undergo keratoprosthesis find that they can reduce their reliance on visual aids such as glasses or contact lenses, leading to greater independence and improved quality of life.
Enhanced Ocular Comfort: Keratoprosthesis can alleviate discomfort associated with severe corneal diseases, such as chronic pain, irritation, and light sensitivity, allowing patients to enjoy greater comfort and well-being.
Expanded Treatment Options: For individuals who have exhausted traditional treatment options such as corneal transplantation or contact lenses, keratoprosthesis offers a viable alternative for restoring vision and improving ocular function.
Long-Term Solution: Unlike some temporary treatments or interventions that may provide short-term relief, keratoprosthesis offers a durable, long-term solution for patients with irreversible corneal conditions, providing sustained improvement in vision and quality of life.
Potential for Improved Social and Professional Engagement: By enhancing visual function and reducing the impact of corneal diseases on daily activities, keratoprosthesis can empower patients to engage more fully in social, professional, and recreational pursuits, leading to a more fulfilling and active lifestyle.
Keratoprosthesis Outcomes
Typical keratoprosthesis outcomes include improved visual acuity, enhanced ocular surface integrity, and restored ocular function in patients with severe corneal diseases or conditions.
However, there are potential risks and complications associated with the procedure, including infection, inflammation, glaucoma, and retinal detachment, which may impact outcomes and require close monitoring and management.
Potential Keratoprosthesis Complications
Infection: Bacterial, fungal, or viral infections can occur following keratoprosthesis surgery, leading to corneal inflammationpain, and potential vision loss if left untreated.
Inflammation: Post-operative inflammation may occur as the body's response to surgery, causing discomfort, redness, and swelling in the eye. Prolonged inflammation can contribute to other complications and hinder visual recovery.
Glaucoma: Elevated intraocular pressure (IOP) can develop after keratoprosthesis surgery, leading to optic nerve damage and irreversible vision loss if not managed promptly. Glaucoma monitoring and treatment are essential to preserve vision.
Retinal Detachment: Retinal detachment, characterized by the separation of the retina from its underlying tissue, is a severe complication that can occur after keratoprosthesis surgery. Symptoms include sudden flashes of light, floaters, and vision loss, requiring urgent intervention to prevent permanent vision impairment.
Corneal Melting: Corneal melting, or the breakdown of corneal tissue, can occur due to various factors such as infection, inflammation, or tissue necrosis. Corneal melting compromises the integrity of the cornea and may lead to device extrusion or displacement if not addressed promptly.
Device Extrusion or Displacement: Improper wound healing or mechanical factors can contribute to the extrusion or displacement of the keratoprosthesis device. This complication requires surgical intervention to reposition or replace the device and restore ocular function.
Keratoprosthesis and Keratoplasty
Keratoprosthesis and keratoplasty are both surgeries that help people with problems in their corneas. Here's a simple breakdown of each:
Keratoplasty: This is like a corneal transplant. It's when a surgeon removes the damaged or diseased part of the cornea.A healthy cornea from a donor replaces it. It's like replacing a broken piece of glass with a new one. Keratoplasty helps improve vision and eye health for people with issues like corneal scars or thinning.
Keratoprosthesis: This is a bit different. Instead of using a donor cornea, a keratoprosthesis surgery involves placing an artificial cornea into the eye. It's like putting in a small, clear window to help people see better when their cornea can't be fixed with a regular transplant. This procedure is usually for people who can't have a regular corneal transplant or have had problems with them in the past.
Recent Advancements in Keratoprosthesis Technology
As technology evolves, so does the landscape of keratoprosthesis. Advancements aim to enhance efficacy, durability, and patient outcomes.
The Boston Type II Keratoprosthesis
The Boston Type II Keratoprosthesis is an improved version of the Boston Type I. It has a longer optic that goes through a hole in the upper eyelid. This modification facilitates its utility in managing the most severe cicatrizing ocular surface diseases.
Latest Novel Device for keratoprosthesis
The latest novel device for keratoprosthesis implantation incorporate advancements in materials, design, and surgical techniques to enhance safety, efficacy, and long-term outcomes. These devices may offer improved biocompatibility, tissue integration, and stability compared to traditional methods, potentially leading to better visual outcomes and reduced complications.
Summary
To summarize, advancements in keratoprosthesis (Kpro) implantations have significantly expanded treatment options for individuals grappling with complex corneal conditions such as autoimmune diseases and corneal melt.
The evolution of surgical techniques, including the innovative osteo-odonto-keratoprosthesis (OOKP), has paved the way for enhanced visual rehabilitation and restored vision in patients where traditional methods may have fallen short.
Clinical trials, supported by organizations like the American Academy of Ophthalmology, continue to explore novel approaches to improve vision outcomes and mitigate complications such as retinal detachments.
Through the judicious use of topical antibiotics, eye drops, and even soft contact lenses, the landscape of ophthalmic care is continuously evolving to offer hope and tangible solutions for those facing the challenges of severe corneal diseases.