- Immune Checkpoint Inhibitors and Their Side Effects - (https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/immunotherapy/immune-checkpoint-inhibitors.html)
- Checkpoint Inhibitors - (https://www.mskcc.org/cancer-care/diagnosis-treatment/cancer-treatments/immunotherapy/checkpoint-inhibitors)
- About Checkpoint Inhibitors - (https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/immunotherapy/types/checkpoint-inhibitors)
- Immune Checkpoint Inhibitors - (https://www.mdanderson.org/treatment-options/immune-checkpoint-inhibitors.html)
- Why Immunotherapy? A Targeted Answer to Cancer - (https://www.cancerresearch.org/en-us/immunotherapy/why-immunotherapy)
- Cancer Immunotherapy - (https://www.immunology.org/sites/default/files/Cancer%20Immunotherapy.pdf)
- About Immune checkpoint inhibitors - (https://www.whatisbiotechnology.org/index.php/science/summary/checkpoint-inhibitor/immune-checkpoint-inhibitors-are-key-cancer-treatment-tool)
- Baraibar I, Melero I, Ponz-Sarvise M, Castanon E. Safety and Tolerability of Immune Checkpoint Inhibitors (PD-1 and PD-L1) in Cancer. Drug Saf. 2019 Feb;42(2):281-294. doi: 10.1007/s40264-018-0774-8. PMID: 30649742. - (https://www.immunology.org/sites/default/files/Cancer%20Immunotherapy.pdf)
- Huang XZ, Gao P, Song YX, Sun JX, Chen XW, Zhao JH, Wang ZN. Efficacy of immune checkpoint inhibitors and age in cancer patients. Immunotherapy. 2020 Jun;12(8):587-603. doi: 10.2217/imt-2019-0124. Epub 2020 May 7. PMID: 32378444. - (https://www.immunology.org/sites/default/files/Cancer%20Immunotherapy.pdf)
- Robert, C. A decade of immune-checkpoint inhibitors in cancer therapy. Nat Commun 11, 3801 (2020) - (https://doi.org/10.1038/s41467-020-17670-y)
- Tan S, Li D, Zhu X. Cancer immunotherapy: Pros, cons and beyond. Biomed Pharmacother. 2020 Apr;124:109821. doi: 10.1016/j.biopha.2020.109821. Epub 2020 Jan 18. PMID: 31962285. - (https://doi.org/10.1038/s41467-020-17670-y)
- Shweta Joshi, Donald L. Durden, "Combinatorial Approach to Improve Cancer Immunotherapy: Rational Drug Design Strategy to Simultaneously Hit Multiple Targets to Kill Tumor Cells and to Activate the Immune System", Journal of Oncology, vol. 2019, Article ID 5245034, 18 pages, 2019 - (https://doi.org/10.1155/2019/5245034)
- Immunotherapy: Precision Medicine in Action - (https://www.hopkinsmedicine.org/inhealth/about-us/immunotherapy-precision-medicine-action-policy-brief.html#:~:text=15%2D20%25%20of%20patients%20achieve%20durable%20results%20with%20immunotherapy)
- How Often Do You Receive Immunotherapy? - (https://moffitt.org/treatments/immunotherapy/immunotherapy-faqs/how-often-do-you-receive-immunotherapy/)
- Tumor Mutational Burden - (https://www.cancer.gov/publications/dictionaries/cancer-terms/def/tumor-mutational-burden)
- What is Pharmacovigilance? - (https://www.who.int/teams/regulation-prequalification/regulation-and-safety/pharmacovigilance)
- Microsatellite Instability - (https://www.cancer.gov/publications/dictionaries/cancer-terms/def/microsatellite-instability)
What are Immune Checkpoint Inhibitors?
Immune Checkpoint Inhibitors are a kind of medication that blocks checkpoint proteins to treat Cancer. They are a class of Immunotherapy that use monoclonal antibodies for treatment and were first discovered in 1995 by Jim Allison, Ph.D.
How Do Immune Checkpoint Inhibitors Work Against Cancer?
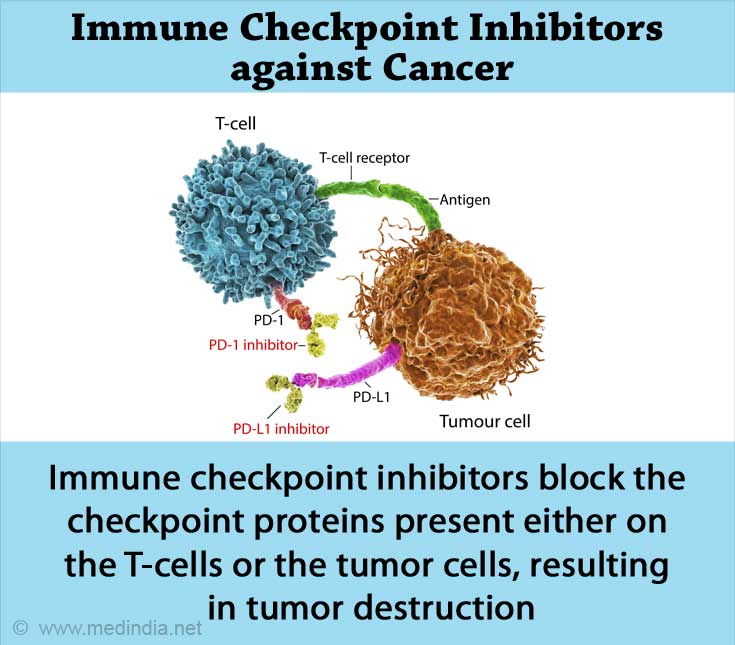
The T-lymphocytes are central to the immune system and play a vital role in generating immune responses against infections and tumors. The activity of T-cells against tumor cells is regulated by some proteins called 'Checkpoint proteins.' These proteins are present either on the T-cells or on the tumor cells.
Normally when the immune checkpoint proteins interact with their ligands or molecules (ligand from Latin, means “tie or bind”), T-cells get an "off" signal. This stops them from destroying the cancerous cells, leading to an overgrowth of tumor cells. The primary function of these proteins is to keep the immune response under control. Still, Cancer cells sometimes use these proteins as their chances of escape from being eliminated.
Here is where ‘Immune Checkpoint Inhibitors’ come into play. These molecules block the immune checkpoints, preventing the "off" signal from being sent to the T-cells. Thus, T-cells can now kill the cancer cells.
There are three main kinds of checkpoints in our immune system, namely:
- CTLA-4 (Cytotoxic T lymphocyte-associated protein-4)
- PD-1(Programmed cell death protein-1)
- PD-L1 (Programmed cell death-Ligand 1)
What are the Types of Immune Checkpoint Inhibitors?
Immune Checkpoint Inhibitors are classified based on their target proteins. Based on that, there are three kinds of Checkpoint Inhibitors as follows:
- CTLA-4 inhibitors
- PD-1 inhibitors
- Pembrolizumab (Keytruda)
- Nivolumab (Opdivo)
- Cemiplimab (Libtayo)
- PD-L1 inhibitors
- Atezolizumab (Tecentriq)
- Avelumab (Bavencio)
- Durvalumab (Imfinzi)
Which Cancers are Treated with Immune Checkpoint Inhibitors?
Immune Checkpoint Inhibitors are generally used in the form of intravenous drip into our bloodstreams.
As per the current FDA indications, they are used to treat a variety of cancers including,
- Breast cancer
- Cervical cancer
- Colorectal cancer
- Endometrial cancer
- Head and neck squamous cell cancer
- Hepatocellular carcinoma
- Hodgkin lymphoma
- Melanoma
- Non-small cell lung cancer
- Renal cell carcinoma
- Small cell carcinoma
- Urothelial carcinoma

Clinical Efficacy and Safety of Immune Checkpoint Inhibitors
The efficacy of Immune checkpoint inhibitors depends on the types and quantity of expression of biomarkers in the patient's body. The other factors considered are:
- Stage of the Cancer
- Type of the Cancer
- Treatment history
- Tumor mutation burden (TMB)
- Microsatellite instability (MSI)
The clinical efficacy of PD-1 / PD-L1 inhibitors is approximately 80 % in lymphoma, 60 % in high microsatellite instability (MSIH) tumors. Their efficacy in treating other common solid tumors ranges between 10 % and 30 %.
The safety profiles of checkpoint inhibitors are better when compared to the traditional cytotoxic agents for cancer treatment. Lower toxicity and better tolerability are seen in a majority of cancer patients when compared to chemotherapy medications.
On the other hand, experts say that the treatment with immune checkpoint inhibitors could create a unique set of adverse effects that might not be seen with traditional chemotherapy agents. Although the treatment option seems to trigger manageable side effects, the area is still under research.
Some recent case studies and pharmacovigilance investigations report serious adverse effects, especially related to lungs and gastrointestinal system in the patients under checkpoint inhibitor therapy.
What are the Pros and Cons of Immune Checkpoint Inhibitors?
Although immune checkpoint inhibitors are a breakthrough in oncology, they have their own pros and cons, like any other treatment options.
The advantages of using Immune checkpoint inhibitors for cancer therapy include:
- Immune checkpoint inhibitors can work effectively against many different cancers. These drugs converted many "fatal" and "difficult-to-treat" cancers into "curable" ones.
- They work exclusively against malignancies, and so, they do not cause side effects as seen in the traditional, non-specific treatments like chemotherapy and radiation. Side effects of checkpoint inhibitors are becoming more manageable.
- They offer a long-term decrease in or disappearance of signs and symptoms of Cancer.
- Ultimately, as the immune checkpoint inhibitors join hands with our immune system to cope with Cancer, the likelihood of cancer recurrence is greatly reduced.
The major disadvantages of checkpoint inhibitors are:
- The hyperactive T-cells that have got an immune boost could possibly damage normal cells. The side effects include diarrhea, inflammation of internal organs, and skin rashes.
- The long-term adverse effects of checkpoint inhibitors that can affect vital organs are yet to be explored.
- The immune checkpoint blockade triggered through the use of checkpoint inhibitors leads to autoimmune reactions in the body.
- The treatment with these drugs is expensive and poses a significant burden on both patients and healthcare professionals.
As the cancer cells not only inhibit pathways that affect T cell functions but also have other mechanisms to multiply themselves, the patient might need combination therapies to combat the underlying malignancy. This could lead to serious adverse effects due to drug-drug interaction, making the management of side effects costly again.