- About Pancreas transplant - (http://www.nhs.uk/conditions/pancreastransplant/pages/introduction.aspx)
- What is the pancreas? - (http://pathology.jhu.edu/pc/basicoverview1.php?area=ba)
- Risks-Pancreas transplant - (http://www.nhs.uk/conditions/pancreastransplant/pages/riskspage.aspx)
- Transplantation - (https://www.kidney.org/atoz/content/pancreastx)
- Pancreas transplant - (http://www.mayoclinic.org/tests-procedures/pancreas-transplant/basics/definition/prc-20014239)
- Pancreas Transplant Treatments and Procedures - (http://www.pennmedicine.org/transplant/patient-care/transplant-programs/pancreas-transplant/transplant-process/)
- Information About Pancreas transplant - (http://www.mayoclinic.org/tests-procedures/pancreas-transplant/basics/results/prc-20014239)
What is Pancreas Transplantation?
The pancreas is a gland located in the abdomen lying between the stomach and spine. The main function of pancreas is to synthesize insulin, a hormone used for regulating sugar (glucose) absorption into cells.
In Type 1 diabetes the pancreas is not able to make enough insulin causing the blood sugar to rise dangerously.
In most of the cases, pancreas transplants are done along with kidney transplants, but in some cases done alone too.
A pancreas transplant is usually recommended only if the person has difficulty controlling diabetes with standard treatment. People who do not respond well to insulin treatment and have associated complications are usually put on the transplant list.
Pancreas usually comes from a deceased donor. However sometimes partial pancreas donation is also possible from a living donor. Sometimes, instead of transplanting whole or partial pancreas, a big group of pancreas islet cells (responsible for making insulin) are transplanted. The islet cells are normally injected directly into the liver, where insulin production begins. As these cells can make insulin, it takes on the function of the pancreas.
Pancreas transplant has a range of side effects including rejection, thrombosis (blood clots), pancreatitis (inflammation), abdominal abscess and infections. This procedure is only considered if all other treatment options have been exhausted.
Procedure
Steps:
- Evaluation
- Preparing for Transplant
- Transplant surgery
- After transplant care
Evaluation
Before the transplant, members of the transplant team evaluate the safety and benefits of the procedure. Evaluation process usually lasts for three days and may include:
- Physical Examination
- Blood tests which include analysis of blood and tissue types
- Imaging tests
- Cardiac Catheterization
- Echocardiogram and other heart testing
- Specialist consultations with Endocrinologists, Cardiologists, pancreas transplant specialists and other required specialists
Preparing for Transplant
Once approved for a pancreas transplant, the receiver will be kept on a waiting list for a donor. Close contact with transplant team is essential and the transplant coordinator has to be notified of any significant changes in medical condition.
Preparation should be made to get to the hospital quickly, within 8 to 12 hours, after receiving notice about the pancreas availability. General health should be well maintained during this time.
Transplant Surgery
Before transplant, blood tests are done to ensure that the receiver’s tissue is compatible with potential donor’s organ tissue and to check for adverse antibodies.
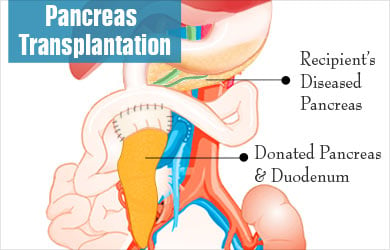
The duration of the surgery is around 3-4 hours. At the time of surgery, the surgeon makes an incision at the centre of the abdomen. Donor’s pancreas and a small part of donor’s intestine is then placed on the right side of pelvis. Pancreas of the receiver is not usually removed as it aids in digestion. Donor’s pancreas is connected to blood vessels that supply blood to legs and the small portion of adjacent donor intestine is connected to small intestine. The transplanted pancreas immediately starts functioning and insulin needs are minimal if any.
After Transplant Care
Once the transplant is done, the patient is required to stay in the hospital for about a week. Treatment team will monitor the recovery progress in the hospital. This is done by checking incision area, assisting in pain management, aiding emotional concerns, educating on further processes, adjusting insulin if needed and checking if there are any signs of complications or rejections.

Post-transplant Outlook
With the new pancreas, the patient will no longer require insulin therapy. However, the patient will have to take several precautions to avoid infection and rejection as the host immune system may reject the donor pancreas. Some of the other medications include immunosuppressants antiviral and antibacterial medications.







