Two people in the US, who underwent lung transplantation, have been infected with a deadly bacteria, according to the Centers for Disease Control and Prevention.

Suspected Legionella Transmission from a Single Donor to Two Lung Transplant Recipients - Pennsylvania, May 2022
Go to source).
Legionnaires Disease Outbreak: CDC Investigates Cases Linked to Lung Transplant from Common Donor
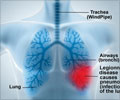
Legionnaires disease is a severe pneumonia caused by Legionella bacteria. Comorbidities, including recent organ transplantation, increase the risk for infection. The CDC in its latest Morbidity and Mortality Weekly Report (MMWR) detailed two cases of Legionnaires disease (2✔ ✔Trusted SourceAbout Legionnaires Disease and Pontiac Fever
Go to source) from Pennsylvania in June 2022 in patients who received a lung transplant from the same donor. The donor, a man aged 30-39 years, died after drowning in a river, raising suspicion of potential donor-derived transmission, because Legionella bacteria naturally live in freshwater. The first Legionnaires disease case was identified in a woman aged 70-79 years who received a right lung transplant in May 2022. Nine days after transplantation, the patient’s laboratory results revealed an elevated white blood cell count and acute anemia, which prompted imaging studies. A computed tomography (CT) scan identified dense consolidation in the middle lobe of the donor lung, which evolved into a cavitary lesion during the subsequent week. After treatment the patient fully recovered. The second case occurred in a man aged 60-69 years (patient B) who received a left lung transplant on the same day and from the same donor. Patient B experienced multiple postoperative complications, including the need for extracorporeal membrane oxygenation and renal replacement therapy, and he received antibiotic treatment with doxycycline starting on postoperative day 15.
‘While solid organ transplants heighten Legionella infection risk due to necessary immunosuppressive therapy, organ-to-organ transmission had not been previously reported. Swift detection remains crucial in limiting harm and fatalities in transplant recipients. #transplant #bacterialinfection ’





A nonspecific sign that might represent infection were noted in the donor lung after a CT scan performed 24 days after transplantation. Although the patient experienced an initial clinical recovery, after a prolonged hospital stay, he died approximately six months after the transplant surgery due to respiratory failure secondary to a mucous plug.Doctors also tested three other people who received heart, liver, and right kidney, from the same donor, but they remained free of the bacteria. After learning about the infections, the Pennsylvania Department of Health went on the hunt for the source of the bacteria.The department tested the water at the hospital where the transplant operations were done but did not find any evidence of Legionella. But the presence of different Legionella species in the two patients can potentially be explained by infections derived from the donor’s exposure to river water, which might contain a larger diversity of Legionella species compared with potable water, they said.
Legionella bacteria are found naturally in freshwater environments, can survive under a wide range of environmental conditions, and typically grow best in warm water at temperatures of 25 degrees Celsius - 45 degrees Celsius. An effective water management programme, along with strict adherence to infection control guidance, remain the best means to prevent health care-associated Legionnaires disease.
References:
- Suspected Legionella Transmission from a Single Donor to Two Lung Transplant Recipients - Pennsylvania, May 2022 - (https://www.cdc.gov/mmwr/volumes/72/wr/mm7237a1.htm)
- About Legionnaires Disease and Pontiac Fever - (https://www.cdc.gov/legionella/about/index.html)
Source-IANS