A review article states that fibromyalgia, has seen many recent evolutions regarding its diagnosis and management which should instil new approaches.

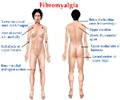
Fibromyalgia, recognized as a medical condition in 1990 by the American College of Rheumatology classification, has been associated with skepticism about its validity as a medical condition because of its non-specific nature — pain, sleep disturbance, fatigue and mood disruptions — and the inability to confirm the diagnosis with clinical or laboratory tests.
Because fibromyalgia cannot be diagnosed by any laboratory test, unnecessary investigations should be avoided. "In the absence of a confirmatory test, expert opinion suggests that investigations should be limited to simple blood tests, including a complete blood count, erythrocyte sedimentation rate, C-reactive protein level, thyroid function and creatine kinase level, when an alternative diagnosis is considered," write the authors. Another major shift for fibromyalgia is the elimination of the tender point count, which has been erroneously embedded in the diagnosis of fibromyalgia over the past 20 years.
Although rheumatologists were previously seen as physicians responsible for the diagnosis and management of this condition, the prevalence rate of 3% of the population makes it untenable for most patients to be diagnosed and managed in a specialist setting. Therefore, primary care physicians are best positioned to take over this role, as recommended by the 2012 Canadian Fibromyalgia Guidelines.
The most appropriate management strategy for this condition will be a combination of nonpharmacologic (i.e. exercise, relaxation techniques, cognitive behavioural therapy, etc.) and pharmacologic therapies tailored to the individual patient. The main treatment goal is to improve function by alleviating the most troublesome symptom(s), with pain recognized as the pivot symptom.
"Until the pathogenesis of fibromyalgia has been more clearly established, skepticism about the condition will remain," write the authors. "Even within the limitations of current knowledge, physicians must care for these patients according to the best available evidence and using sound clinical judgement."
Advertisement
Source-Eurekalert