Novel MRI techniques used to target a small area in the brain more accurately tied to Parkinson's disease and essential tremor could lead to better outcomes without surgery and with minimum risk of negative effects of treatment of Parkinson's disease and tremors.
‘Essential tremor affects up to 10 million Americans and Parkinson's disease impacts over 1 million.
’





"The benefit for patients is that we will be better able to target the brain structures that we want," Shah says. "And because we're not hitting the wrong target, we'll have fewer adverse effects." The procedures are already Food and Drug Administration-approved for use in patients, and UTSW plans to begin employing them to treat patients when its Neuro High Intensity Focused Ultrasound Program opens this fall.Adverse effects from imprecise targeting include problems walking or slurring words. While such effects are usually temporary, they can be permanent in 15 to 20 percent of cases, says Dr. Shah.
Essential tremor and Parkinson's disease are neurologic diseases thought to have genetic links. The first line of treatment for the involuntary trembling or shaking seen with these diseases is medication. However, approximately 30 percent of patients do not respond well to drugs, according to the study.
In the late 1990s, neurosurgeons began using a procedure called deep brain stimulation, opening the skull to permanently implant metal electrodes that could then be stimulated via a battery pack.
About a decade ago, a new MRI-guided procedure emerged that uses high-intensity ultrasound waves to heat and eliminate a small section of the thalamus linked to the disorders. MRI-guided HIFU is currently approved for the treatment of essential tremor and tremors seen in Parkinson's disease patients. The outpatient procedure does not require opening the skull, and the patient is awake while it is performed, says Dr. Shah. "No cuts. No anesthesia. No implanted devices."
Advertisement
Traditionally, doctors have relied on either landmarks or maps of the brain drawn from cadavers to help them pinpoint the correct location. However, Dr. Shah says that every brain is different, and tiny errors can lead to damage in surrounding tissue or to missing portions of the correct target.
Advertisement
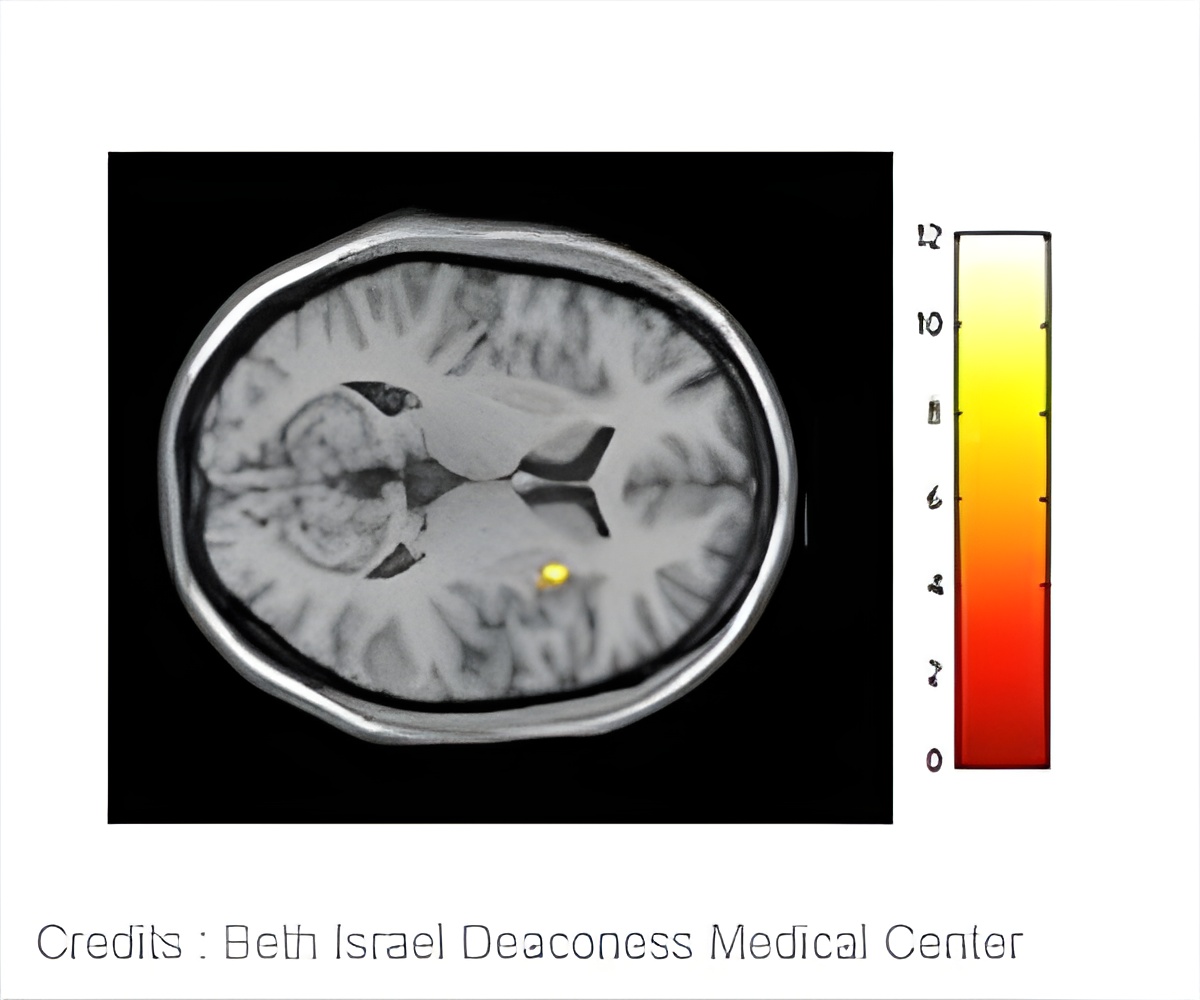
The most widely studied and perhaps most promising imaging method is called diffusion tractography, says Dr. Shah. It creates precise brain images by taking into account the natural water movement within tissues.
The other methods described are quantitative susceptibility mapping - which creates contrast in the image by detecting distortions in the magnetic field caused by substances such as iron or blood - and fast gray matter acquisition TI inversion recovery - which operates much like a photo negative, turning the brain's white matter dark and its gray matter white in order to provide greater detail in the gray matter.
Dr. Shah and his team plan to participate in a multicenter clinical trial with collaborators at the Mayo Clinic in Rochester, Minnesota, testing the diffusion tractography method in patients.
Source-Eurekalert