Human stem cells undergo ageing process and not immune to it state scientists at the Stanford University School of Medicine.
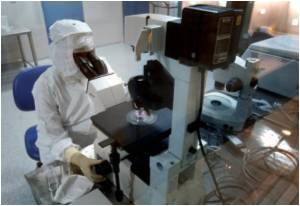
Specifically, the researchers found that hematopoietic stem cells from healthy people over age 65 make fewer lymphocytes — cells responsible for mounting an immune response to viruses and bacteria — than stem cells from healthy people between ages 20 and 35. (The cells were isolated from bone marrow samples.) Instead, elderly hematopoietic stem cells, or HSCs, have a tendency to be biased in their production of another type of white blood cell called a myeloid cell. This bias may explain why older people are more likely than younger people to develop myeloid malignancies.
The study will be published online Nov. 28 in the Proceedings of the National Academy of Sciences. Pang, who is in the Medical Science Training Program at Stanford, is the first author of the research; professor of pathology Irving Weissman, MD, is the senior author. Weissman is also the director of Stanford's Institute for Stem Cell Biology and Regenerative Medicine.
Pang began the study to understand whether human HSCs aged like mouse HSCs. Previous studies had shown that mouse HSCs change in number and function as a laboratory mouse grows older. She obtained HSCs from 15 healthy elderly people and 28 healthy young people and compared their prevalence, distribution and cell cycle profile.
She found that HSCs comprised a greater proportion of bone marrow cells in older people than in younger people. They were also more likely to be actively dividing than younger HSCs. But their greater numbers and increased proliferation didn't translate into greater efficiency; like a top wobbling out of control as its rotation slows, the aging HSCs instead appear to be unsuccessfully trying to keep up with the demands of everyday life.
When Pang purified the HSCs and grew them in laboratory dishes, she found that HSCs from older people were less able to differentiate into B lymphocytes and more likely to become myeloid cells. Furthermore, immune-deficient laboratory mice given transplants of older, human HSCs exhibited a higher proportion of myeloid to lymphoid cells in their bone marrow in the weeks to months after the transplant.
Advertisement
Overall, the results mirror those seen in studies of HSCs from laboratory mice of varying ages. They suggest that human HSCs struggle as a person ages, and that this struggle can sometimes lead not only to inadequate immune responses, but also to inappropriate growth and specific types of blood cancers, such as acute myeloid leukemia. They also contribute valuable information for the study of many other conditions.
Advertisement
"These findings will also serve as an important baseline for future studies of age-related diseases, such as myeloid dysplastic syndrome, anemia and leukemia," said Pang. "Now that we know how HSCs change and function in elderly individuals who are not ill, we should be able to tease out disease-associated changes from normal age-associated phenomena."
Source-Eurekalert