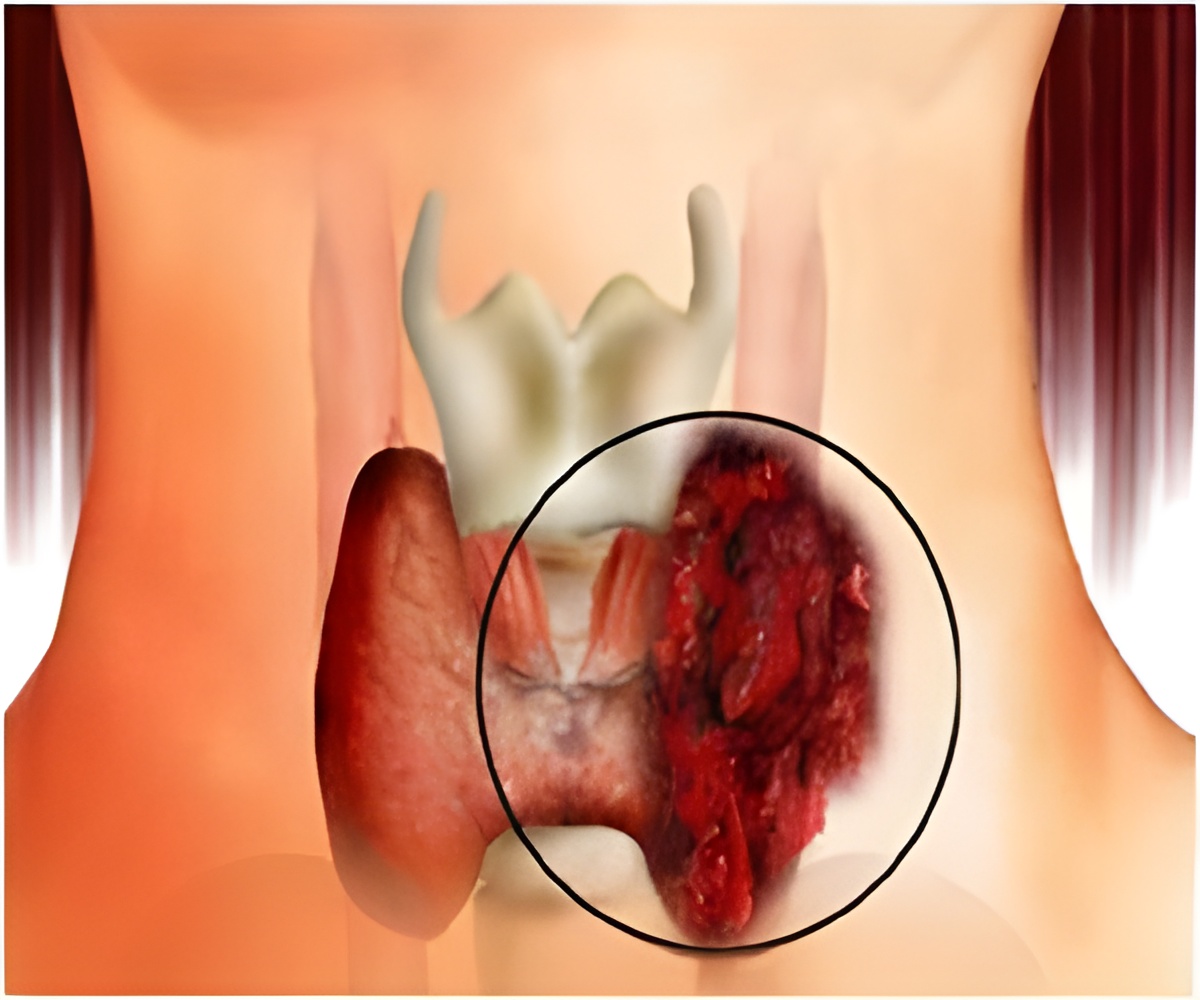
According to a head and neck surgeon at Dartmouth-Hitchcock Norris Cotton Cancer Center, the rapid increase in papillary thyroid cancer in the US, may not be linked to increase in occurrence.
"This work shows that access to health care is an important driver in the rising incidence of thyroid cancer," said Davies. "People with insurance are more likely to be diagnosed with thyroid cancer than those without insurance." In addition researchers found that higher education levels and higher rates of white collar employment were also associated with increased diagnosis rates.
Papillary thyroid cancer is rising 8.8 percent in Americans over age 65 who have Medicare. Among adults under age 65, who do not have access to Medicare, the rate of increase is 6.4 percent. The mortality rate from thyroid cancer, however, has not changed.
"We did the study to understand who is at risk of being diagnosed with thyroid cancer, which is now— like prostate cancer—recognized to be a disease that is commonly over diagnosed," said Davies.
Over diagnosis is the identification of a cancer that would otherwise not have been identified in a person's lifetime.
"The findings are counterintuitive for many: having good health insurance puts you at risk for something bad—the unnecessary identification and treatment of a cancer that was never destined to cause a problem," said Davies.
Advertisement
How will this finding change the practice of medicine? According to Davies, "As a next step we should look to protect patients from unnecessary workups of thyroid findings that do not present a significant threat to their health."