Researchers have found that sorafenib (Nexavar) helps patients with advanced liver cancer live about 44 percent longer compared with patients who did not receive the anti-cancer drug.
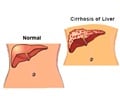
Researchers have found that sorafenib (Nexavar) helps patients with advanced liver cancer live about 44 percent longer compared with patients who did not receive the anti-cancer drug. The findings is a significant advance in the management of liver cancer, which is the third cause of cancer death globally, often resulting in death within a year of diagnosis.
“This is the first time that we’ve had an effective systemic treatment for liver cancer,” said Josep Llovet, MD, Director of Research in Liver Cancer at Mount Sinai School of Medicine in New York, and a Professor at the Barcelona Clinic Liver Cancer (BCLC) Group in Barcelona, Spain and lead author of the study. “Our findings demonstrated survival advantages that are both statistically significant and clinically meaningful.”Sorafenib, a tablet that is taken orally, is approved in the United States for treating a form of advanced kidney cancer, and is currently being evaluated in patients with other cancers. Some 40 percent of liver cancers (and up to 80 percent in Asia and sub-Saharan Africa) are diagnosed at an advanced stage. Therapy for advanced liver cancer may include surgery (if possible), radiation therapy and/or regional chemotherapy (delivered directly into the liver). However, no systemic treatment—anti-cancer medication that enters the bloodstream, either as an oral or intravenous medicine—has proven effective to date for advanced liver cancer.
Dr. Llovet and his associates examined overall survival and the time it took for cancer to grow among patients with previously untreated liver cancer who were randomly assigned to receive either 400 mg of sorafenib twice daily (299 patients) or a placebo (303 patients).
Patients who received sorafenib lived a median of 10.7 months compared with 7.9 months for those who received a placebo. Time to cancer progression was also significantly longer in the treatment group: 5.5 vs. 2.8 months. Due to the positive findings, the study was terminated early.
The incidence of adverse side effects was similar between the two groups (52 percent in the sorafenib group and 54 percent for placebo). The most common moderate to serious side effects were diarrhea (11 percent vs. 2 percent), skin reactions in the hands and feet (8 percent vs. 1 percent), fatigue (10 percent vs. 15 percent) and bleeding (6 percent vs. 9 percent).
Advertisement
KAR