Patients with atrial fibrillation have nearly double the risk of suffering a stroke in the first 30 days after starting to take the anti-clotting drug warfarin compared to non-users, according to a study of over 70,000 patients.

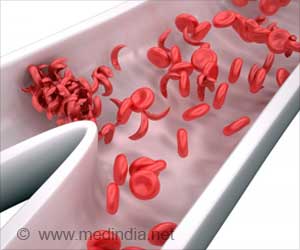
Atrial fibrillation increases the risk of patients suffering a stroke, and warfarin is frequently prescribed for these patients to reduce the likelihood of this happening. However, randomised controlled trials of other anti-clotting drugs have suggested that there might be an increased risk of a stroke at the point when patients move from the trial drugs to warfarin. In addition, it has already been established that there is a possibility that warfarin leads temporarily to a hypercoagulable state – one in which the blood becomes more sticky and more likely to develop dangerous blood clots in the veins or arteries. This is thought to be due to the different effects of warfarin on the production of certain blood clotting factors that are dependent on Vitamin K.
Dr Laurent Azoulay, Assistant Professor in the Department of Oncology at McGill University (Montreal, Canada) and Project Leader at the Centre for Clinical Epidemiology, Lady Davis Institute, Jewish General Hospital in Montreal, led the research. "There is no question that warfarin is highly effective in preventing strokes in patients with atrial fibrillation. Thus, our finding that the initiation of warfarin may be associated with an increased risk of stroke should not deter physicians and patients from using this drug, since this likely affects a small number of patients. Future studies should confirm our results, and identify the small subset of patients who may be at risk. However, the results of our study suggest that physicians should be vigilant when initiating warfarin, particularly in the first week of use," he said.
"An interesting finding was that patients with a history of stroke prior to their atrial fibrillation diagnosis were at higher increased risk of developing a stroke during the initiation of warfarin. This is consistent with the hypothesis that the risk may be highest in patients with hypercoagulable states, which provides insight on the possible biological mechanisms that may be at play in this association.
"To our knowledge, this is the first population-based study to investigate whether the initiation of warfarin is associated with an increased risk of ischaemic stroke – a stroke caused by a blockage in an artery leading to the brain."
The researchers analysed data from 70,766 patients aged 18 or over, who were diagnosed with atrial fibrillation between 1 January 1993 and 31 December 2008. The study was carried out using the UK Clinical Practice Research Datalink, the world's largest primary care database. The researchers followed the patients for up to 16 years until an ischaemic stroke, death, end of registration with their primary care practice or end of the study period, whichever came first.
Advertisement
The researchers believe that the reason for the difference in the effects of warfarin may be that while the drug blocks the activation of clotting factors II, VII, IX and X, it also deactivates two other proteins, C and S, which are anticoagulants. Rapid depletion of protein C, in particular, might lead to a temporary hypercoagulable state.
Advertisement
The researchers hope to repeat the study using databases from other countries and settings.
Source-Eurekalert