Antibiotic treatment changes the gut microbiome that plays an important role in regulating immune system activity that impacts the progression of Alzheimer's disease.
‘The mice treated with high doses of broad-spectrum of antibiotics for six months showed a two-fold decrease in amyloid-ß and a significant elevation in the inflammatory state of microglia in the brain.’





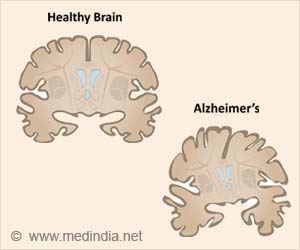
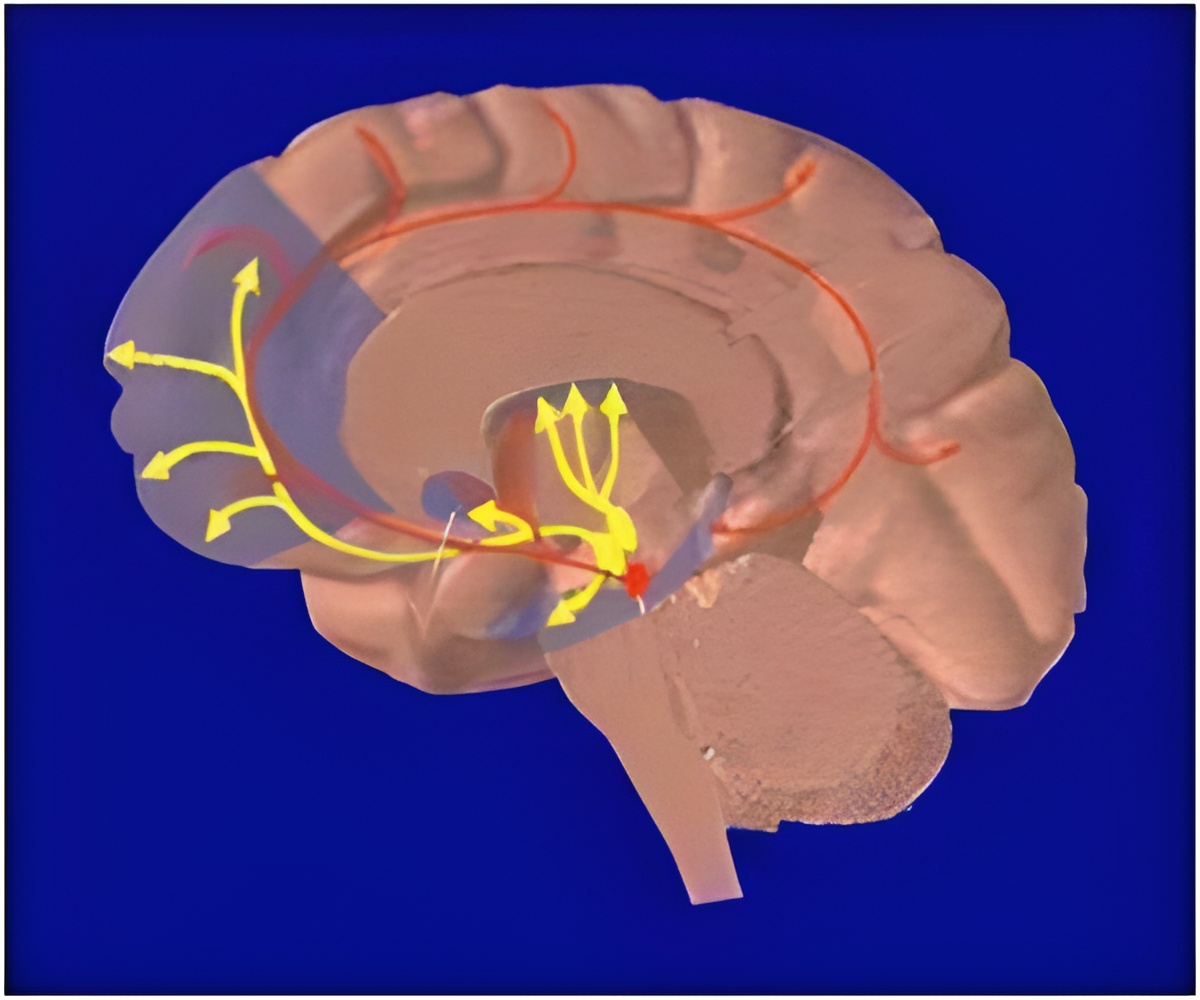
"We're exploring very new territory in how the gut influences brain health," said Sangram Sisodia, PhD, Thomas Reynolds Sr. Family Professor of Neurosciences at the University of Chicago and senior author of the study. "This is an area that people who work with neurodegenerative diseases are going to be increasingly interested in, because it could have an influence down the road on treatments." Two of the key features of Alzheimer's disease are the development of amyloidosis, accumulation of amyloid-ß (Aß) peptides in the brain, and inflammation of the microglia, brain cells that perform immune system functions in the central nervous system. The buildup of Aß into plaques plays a central role in the onset of Alzheimer's, while the severity of neuro-inflammation is believed to influence the rate of cognitive decline from the disease.
For this study, Sisodia and his team administered high doses of broad-spectrum antibiotics to mice over five to six months. At the end of this period, genetic analysis of gut bacteria from the antibiotic-treated mice showed that while the total mass of microbes present was roughly the same as in controls, the diversity of the community changed dramatically. The antibiotic-treated mice also showed more than a two-fold decrease in Aß; plaques compared to controls, and a significant elevation in the inflammatory state of microglia in the brain. Levels of important signaling chemicals circulating in the blood were also elevated in the treated mice.
While the mechanisms linking these changes is unclear, the study points to the potential in further research on the gut microbiome's influence on the brain and nervous system.
"We don't propose that a long-term course of antibiotics is going to be a treatment--that's just absurd for a whole number of reasons," said Myles Minter, PhD, a postdoctoral scholar in the Department of Neurobiology at UChicago and lead author of the study. "But what this study does is allow us to explore further, now that we're clearly changing the gut microbial population and have new bugs that are more prevalent in mice with altered amyloid deposition after antibiotics."
Advertisement
Minter said the collaboration was enabling, and highlighted the cross-disciplinary thinking necessary to tackle a seemingly intractable disease like Alzheimer's. "Once you put ideas together from different fields that have largely long been believed to be segregated from one another, the possibilities are really amazing," he said.
Advertisement
"There's probably not going to be a cure for Alzheimer's disease for several generations, because we know there are changes occurring in the brain and central nervous system 15 to 20 years before clinical onset," he said. "We have to find ways to intervene when a patient starts showing clinical signs, and if we learn how changes in gut bacteria affect onset or progression, or how the molecules they produce interact with the nervous system, we could use that to create a new kind of personalized medicine."
Source-Eurekalert