New studies reveal the promise of engineered bispecific antibodies by demonstrating their power against previously inaccessible tumor cell targets for the first time.

‘New study results highlight the therapeutic potential of bispecific antibodies which, unlike engineered immune cell therapies like CAR T - does not have to be personalized.’
Read More..




Although it is one of the most common mutant tumor suppressor genes known in human cancers, the cancer-related p53 tumor suppressor gene has not been successfully targeted via this approach.Read More..
This is largely because it is much more challenging to reactivate this and other mutant tumor suppressor genes than it is to deactivate cancer-driving genes.
In Science, Emily Han-Chung Hsiue and colleagues successfully engineered a bispecific antibody to reactivate p53. Hsiue et al. first identified a distinct targetable fragment of the mutant tumor suppressor protein and characterized the structural basis for how the fragment is presented to T cells.
They developed an antibody that could recognize this fragment of the mutant p53 protein and that did not cross-react with wild-type p53 in intact cells.
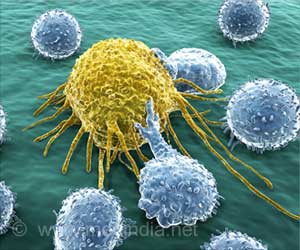
The researchers then converted this antibody into a bispecific antibody format that attaches one portion to mutant p53 antigen on tumor cells and another to a T cell. In mice engrafted with human multiple myeloma cells, the antibody stimulated effective T cell killing of cancer cells that express the mutant p53 protein, resulting in tumor regression.
Advertisement
In Science Translational Medicine, Suman Paul and colleagues employed bispecific antibodies to target malignant T cells in T cell leukemias and lymphomas without harming healthy T cells - a challenging feat in cancer immunotherapy.
Advertisement
Paul et al. hypothesized that targeting the beta chain region of T cell receptors could serve as a potential strategy to selectively eliminate malignant T cells while avoiding collateral damage to healthy T cells.
They engineered bispecific antibodies to home into either TRBV5-5 or TRBV12, two examples of the 30 beta chains that could be present on malignant T cells. They hypothesized that targeting either beta chain could clear cancer cells without harming healthy T cells that express any of the other 29 beta chain variable regions.
In cell lines extracted from patients with T-cell lymphomas and leukemias, application of these bispecific antibodies effectively killed malignant T cells and preserved healthy T cells.
Similarly, in mouse models of human T cell cancers, whereby mice received human T cells via intravenous injection, the antibodies promoted killing of malignant T cells without depleting healthy T cells, leading to major tumor regression.
In Science Immunology, Jacqueline Douglass and colleagues modified bispecific antibodies to recognize and kill tumor cells isolated in culture that bear extremely low levels of cancer-driving mutant RAS proteins on their surfaces. Targeting cancer-driving mutant genes like RAS has emerged as a promising strategy for formulating cancer drugs.
However, the success of this treatment strategy is limited by the fact that some of these cancer-driving mutant proteins are expressed in low levels on tumor cells, making them incredibly difficult to detect - despite their ubiquity in multiple cancer types.
Now, Douglass et al. have used a method called phage display to search for mutant RAS-specific antibodies from a human antibody library. Based on their findings, the researchers developed mutation-associated neoantigen-directed antibodies (MANAbodies) that target mutant RAS neoantigens on tumor cell surfaces. They grafted these mutant RAS-specific MANAbodies onto an optimized T cell-engaging bispecific antibody.
Testing the MANAbody-bearing bispecific antibodies in human lung and pancreatic cancer cell lines, the researchers showed the antibodies could specifically recognize and kill tumor cells that bear extremely low levels of mutated RAS proteins, while having no effect on tumor cells that express wild-type or related mutated proteins.
"Although the studies of Hsuie et al., Douglass et al., and Paul et al. are promising for advancing [bispecific antibodies] into the clinic, there are other factors to consider before therapeutic efficacy can be fully realized," Jon Weidanz says.
For example, he notes that these antibodies are small molecules that can be rapidly cleared from the blood, which will likely make it necessary to continuously infuse these kinds of drugs with an implanted pump or use other methods to extend the drug's persistence in the blood.
Source-Eurekalert