Learn about how autofluorescence imaging allows real-time bacterial identification and offers a significant advancement in managing chronic wounds.
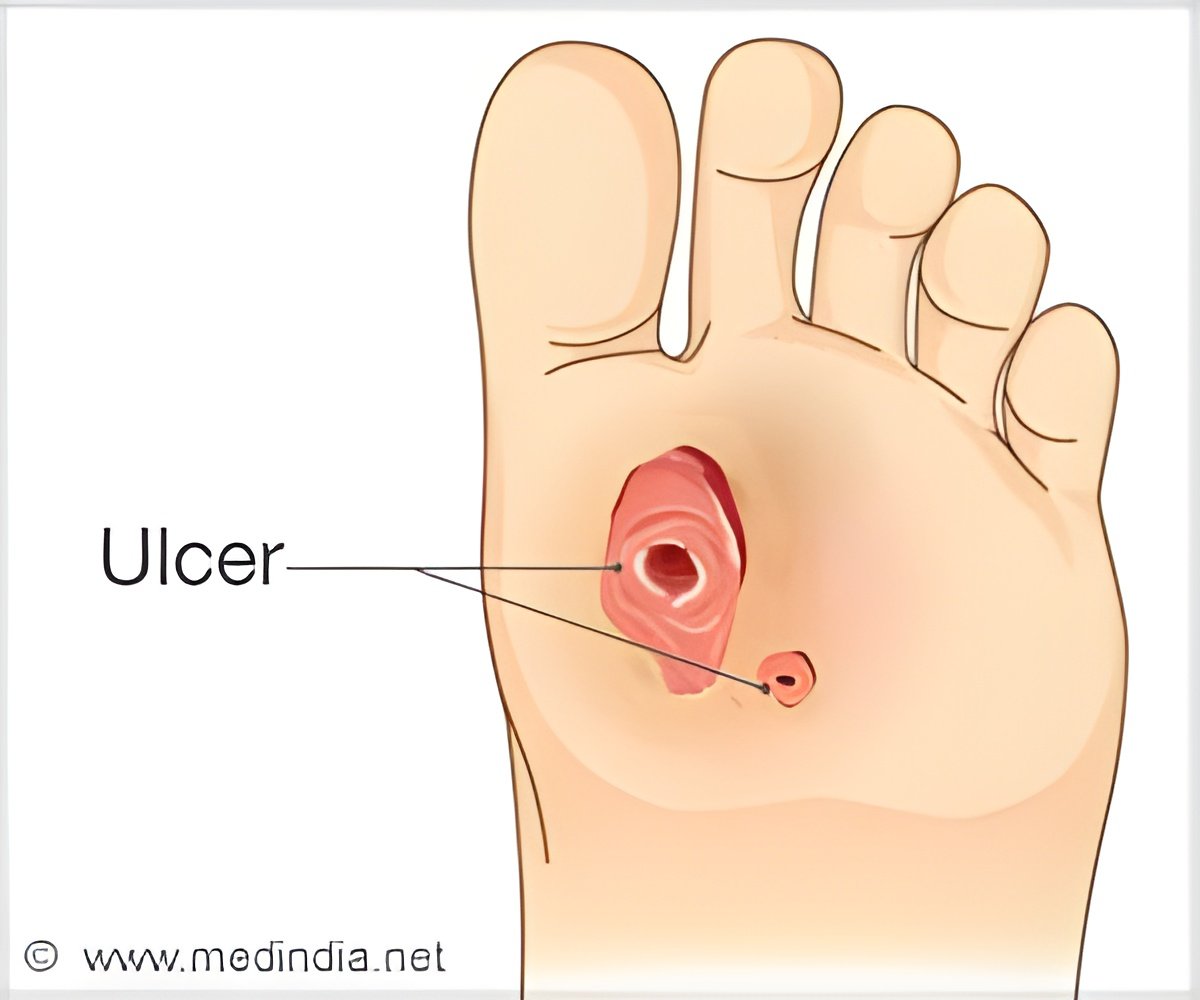
‘According to the American #Diabetes Association, approximately 20% of patients with #diabetic_foot #ulcers require a lower limb amputation.#medindia
’





Autofluorescence Imaging in Bacterial Detection
Autofluorescence (AF) imaging, where a handheld device “lights up” bacteria previously invisible to the human eye, uses violet light to illuminate molecules in the cell walls of any bacteria. Different types of bacteria turn different colors, allowing physicians to immediately determine how much and which types of bacteria are in the wound(1✔ ✔Trusted SourceCurrent and Future Directions in Fluorescence Imaging-Guided Debridement
Go to source).
New Keck Medicine of USC research published in Advances in Wound Care suggests that autofluorescence imaging can be a more effective method to detect bacteria during wound debridement.
"We’re hopeful this new technology can help surgeons improve their accuracy when pinpointing and consequently removing bacteria from wounds and therefore improve patient outcomes, particularly for those with diabetic foot wounds,” said David G. Armstrong, DPM, PhD, a podiatric surgeon and limb preservation specialist with Keck Medicine and senior author of the study. “The early detection and removal of bacteria from a wound is vital to preventing avoidable amputations.”
The research, a literature review of 25 studies examining the effectiveness of AF imaging in treating diabetic patients with foot ulcers, reveals that AF imaging can identify bacteria in wounds in approximately 9 in 10 patients that traditional clinical assessments miss.
Standard Wound Debridement
Traditionally, physicians debride wounds and then send tissue samples to the lab to identify specific types of bacteria present in the wound and determine the best treatment protocol based on those findings, such as starting the patient on antibiotics or providing a special type of wound dressing. This process can take days, during which time an infection can set in, said Armstrong.Advertisement
Another benefit to the technology is that if bacteria is caught early, the patient may avoid being prescribed antibiotics, which in wound care can be prolonged, thus avoiding possible antibiotic resistance.
Advertisement
Keck Medicine physicians are already using the technology to successfully treat patients with chronic wounds, including diabetic foot ulcers.
“I look forward to more research in this area as we hope to see AF imaging become the standard of care for wound care shortly,” said Armstrong.
Reference:
- Current and Future Directions in Fluorescence Imaging-Guided Debridement - (https:www.liebertpub.com/doi/10.1089/wound.2024.0067)
Source-Eurekalert










