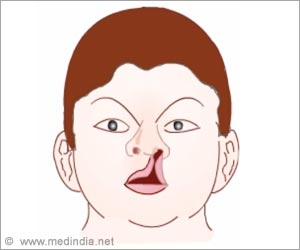
Patients rely on charitable care outside the centralized healthcare system, as a result, surgical treatment of cleft lip and palate is delayed.

"Patients rely on charitable care outside the centralized healthcare system," according to the report by Dr. William Magee III of University of Southern California and colleagues. "As a result, surgical treatment of cleft lip and palate is delayed beyond the standard optimal window compared to more developed countries."
Study in Vietnam Gives New Insights into Barriers to Cleft Lip and Palate Surgery in LMICs
Dr. Caroline Yao and her research team surveyed approximately 450 Vietnamese families seeking cleft lip and/or palate repair surgery for their affected child. The families were seen at four medical missions sponsored by Operation Smile, Inc. Parents were asked in-depth questions about their perceptions of the barriers to surgical and medical care for their child's condition.
At the time of initial cleft surgery, the children's average age was 3.25 years. By comparison, in developed countries, the recommended age for cleft lip and palate repair surgery is between three and 18 months.
Nearly three-fourths of the families had health insurance coverage. Yet 83 percent had their surgery performed by a charitable organization, outside of the national healthcare system.
Advertisement
The survey revealed a wide range of structural, financial and cultural barriers to cleft care. Structural barriers included lack of trained medical personnel, equipment, and medicine. Financial barriers were identified as not only the cost of the surgery, but the cost of travel to obtain care. Cultural barriers included family members' opinions/permission and lack of trust in the medical system/personnel.
Advertisement
People living in LMICs continue to face substantial barriers to accessing healthcare--especially for specialized care such as surgery. Improving access to surgical care has become a major global health priority. However, the current knowledge gap on providing surgery in LMICs, including the need for specialized facilities, physicians, and follow-up care, has only begun to be studied.
The study suggests that charitable missions remain a critical source of access to surgical care in LMICs, even in countries with near-universal health insurance. Based on their findings, Dr. Magee and colleagues propose a new "Surgical LMIC" model to give a more complete picture of the unique barriers to accessing surgery in resource-poor countries--especially for conditions that require multiple operations, as is often required in reconstructive surgery.
"[Our study] also highlights the challenges and successes for mission-based care and the need to better understand surgical barriers in order to design more effective programs for both missions-based and locally sustainable surgical care," Dr. Magee and coauthors write. "Plastic surgeons are uniquely positioned to lead the surgical community in addressing the need for improvements in global surgical access and care, given our history of mission-based work, access to multicultural patients and dedication to education systems within global surgery."
Source-Eurekalert