Basal insulin analogs have revolutionized diabetes care, and especially the treatment of type 2 diabetes, enabling patients to achieve better control
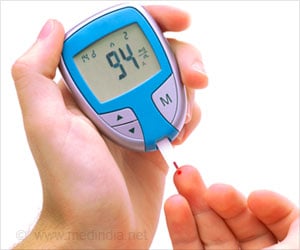
Basal insulin analogs have revolutionized diabetes care, and especially the treatment of type 2 diabetes, enabling patients to achieve better control of blood glucose levels while reducing hypoglycemic episodes. These revolutionary, long-acting basal insulin analogs, intended to replace the natural insulin missing in diabetes, and infusion pumps that provide subcutaneous, continuous delivery of insulin to mimic the function of a normal pancreas, are described in a special supplement to
Diabetes Technology & Therapeutics, a peer-reviewed journal.
More than 25 million people in the U.S. have diabetes, and the global diabetes epidemic is estimated to affect nearly 440 million people by 2030. "The development of basal insulin analogs has greatly impacted the management of diabetes," writes Satish Garg, MD, Editor-in-Chief of
Diabetes Technology & Therapeutics and Professor of Medicine and Pediatrics at the University of Colorado Denver, and Emily Moser, University of Colorado Denver School of Medicine, in their Editorial introducing the broad scope of articles in this issue that detail the history, current status, and clinic promise of ongoing advances in basal insulin analogs and insulin delivery devices.
The controversial role postprandial glucose (PPG)— spikes in blood sugar levels after eating—plays in overall hyperglycemia and in the development of diabetes complications in patients with type 2 diabetes is the focus of an article by Louis Monnier, MD, Claude Colette, PhD, and David Owens, MD, University of Montpellier (France) and University Hospital Llandough (Cardiff, United Kingdom), entitled "Postprandial and Basal Glucose in Type 2 Diabetes: Assessment and Respective Impacts."
Geremia Bolli, MD, Anna Marinelli Andreoli, MD, and Paola Lucidi, MD, PhD, University of Perugia (Italy), review the critical role of basal insulin in maintaining normal blood glucose levels and explain the importance of optimizing basal insulin substitution in individuals with type 1 diabetes. The authors explore the advantages and limitations of the most recent options for basal insulin substitution, including long-acting insulin analogs and continuous subcutaneous insulin infusion. In the article "Optimizing the Replacement of Basal Insulin in Type 1 Diabetes Mellitus: No Longer an Elusive Goal in the Post-NPH Era," the authors conclude that modern physiological basal insulin replacement, combined with other standards of care and patient and physician education, make optimal blood sugar and HbA1c control a realistic target of diabetes management.
In their Concluding Remarks on "The Future of Basal Insulin Supplementation," Airin Simon, MD and J. Hans DeVries, MD, PhD, Academic Medical Centre (Amsterdam, The Netherlands), preview and compare the basal insulin analogs and patch pumps for subcutaneous insulin delivery that are now in development. The results of ongoing clinical studies are promising, but final trial results (being presented at the American Diabetes Association's annual meeting this week in San Diego) are needed to confirm their safety, efficacy, and cost effectiveness.
Source-Eurekalert