Major bleeding after minimally invasive PAD treatment was found to increase the risk of death, revealed new study.
‘For clinicians engaged in the care of patients with lower extremity peripheral artery disease (PAD), the study represents an opportunity to establish best practices and improve patient outcomes: it is time to stop the bleeding.’





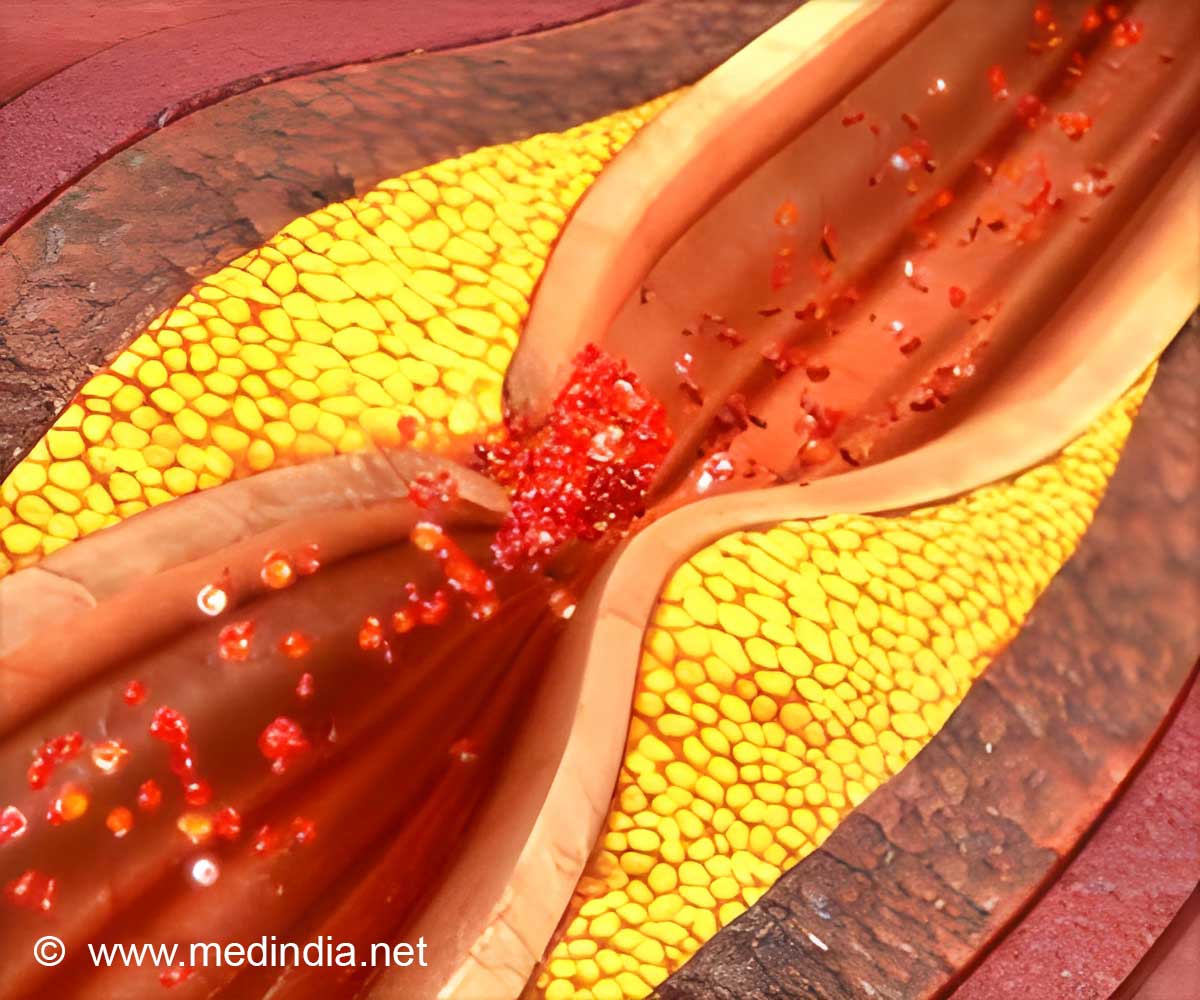
Peripheral vascular intervention (PVI) is a minimally invasive outpatient procedure used to treat peripheral artery disease (PAD), which causes plaque buildup in the arteries leading to the intestines, head, arms and most commonly the legs. PAD affects approximately 8 million Americans.
The goal of PVI is to restore the flow of blood to the lower extremities, eliminating pain, numbness or need for amputation. The procedure involves using a balloon-tipped catheter and/or stents to open blockages from inside the vessel. Over the past two decades, there has been a rapid growth in the use of PVI for the treatment of PAD, but there are limited data about the safety outcomes of PVI in routine clinical practice, Salisbury said. The researchers studied patients undergoing PVI at 76 hospitals in the NCDR PVI Registry from 2014 to 2016. Among 18,289 PVI procedures, major bleeding occurred in 744 (4.1 percent). The in-hospital death rate was higher in patients who experienced bleeding compared with those who did not (6.6 percent vs. 0.3 percent).
The study found patient characteristics associated with bleeding included age, female sex, heart failure and anemia. Patients with resting leg pain or ulcerations due to poor blood flow were also at higher risk. The researchers found certain surgical strategies were associated with bleeding, such as placing the catheter in an artery other than the femoral artery. The use of thrombolytic ("clot-busting") therapy was also associated with an increased risk of bleeding.
"The findings suggest we can use different procedural strategies, such as using different access points for the catheter, alternative blood thinners or different sizes of equipment, to reduce the risk of bleeding," Salisbury said. "We can use the findings to identify factors and create models to predict who is at higher risk of bleeding. In these patients, we need to be especially careful to avoid doing anything that could increase the risk of bleeding."
In an editorial accompanying the study, Douglas E. Drachman, MD, of Massachusetts General Hospital and Beau M. Hawkins, MD, of the University of Oklahoma Health Sciences Center, wrote that the study "demonstrates that bleeding is a common complication of PVI and that bleeding confers significant clinical risk.”
Advertisement











