Single cells in the innermost layer of blood vessels proliferate after injury and in so doing make a significant contribution to the formation of new vessels.
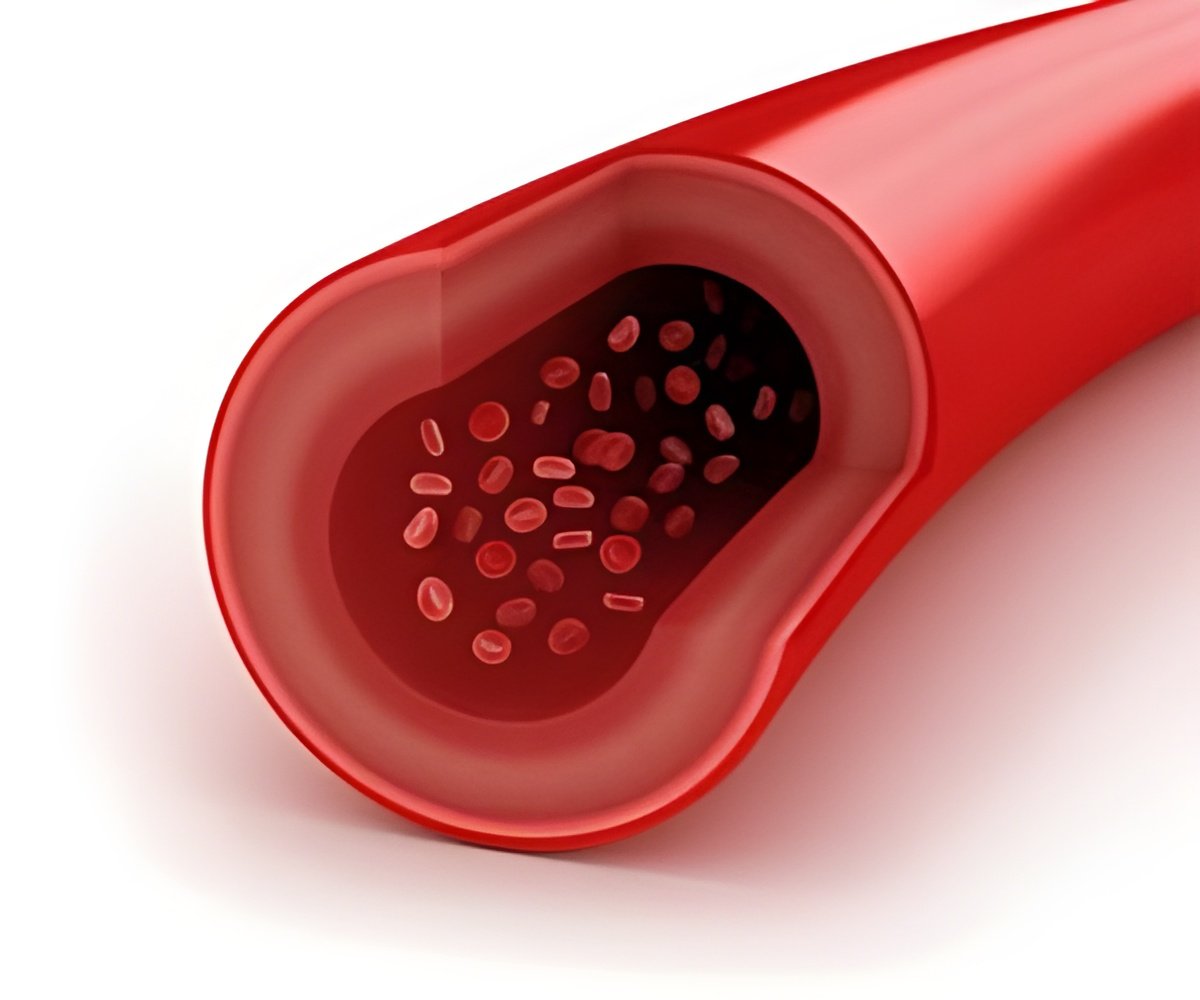
‘Single cells in the innermost layer of blood vessels proliferate after injury and in so doing make a significant contribution to the formation of new vessels.’





In the models used, only endothelial cells fluoresced in three different colors. Since the cells continue to fluoresce when they divide, single endothelial cells and their "progeny" can be tracked. In so doing, the scientists sought to answer the question of whether cell division in the formation of new blood vessels, as known from zebrafish, takes place more or less randomly or whether specific cells divide again and again to produce new vessels. Clonal expansion after a heart attack
In damaged heart tissue following a heart attack, the researchers were able to observe that certain cells had divided repeatedly. They also detected this cell division, which is referred to as clonal expansion, in damaged tissue in skeletal muscles caused by ischemia. To do so, they analyzed the fluorescence in endothelial cells in tissue slices taken from the damaged areas. They found the ratio of clonally expanding cells - between 30 and 50 percent - very surprising. "But perhaps we're even underestimating the ratio of clonal expansion," presumes Dimmeler. "Because after all we haven't conducted a three-dimensional analysis but instead identified the fluorescing cells in two-dimensional tissue slices." In addition, further experiments showed that the vessels formed through clonal expansion are also supplied with blood and thus able to function. In new-born models, by contrast, Professor Dimmeler and her team did not observe any clonal expansion in the formation of new vessels in the retina. It would therefore seem that the growth of blood vessels during normal development results from the random multiplication and integration of cells. This result coincides with observations in zebrafish, in which what is known as "cell mixing" also plays an important role in the formation of new blood vessels during development.
Cell profiling
The researchers were keen to characterize the dividing cells more precisely and to this purpose they analyzed which genes are transcribed in single examples of the clonally expanding endothelial cells. "Surprisingly, we found a large number of gene products that are typical for the transition from an endothelial to a mesenchymal cell," says Dimmeler. This transition, or EndMT process, is a contributor in many pathogenic processes, such as scarring or arteriosclerosis. In endothelial cells, the gene products typical for EndMT do not, however, mirror a transition but instead presumably just an intermediate stage that enables the cells to detach themselves from the cell assembly in order to multiply.
Advertisement
Dimmeler and her team now want to find out what happens with the clonally expanded cells in the long term, since at present they are only able to track their fate for about two months. "We want to know what has happened to these cells after a year and whether the new blood vessels are just as good as the old ones in the long term," says Dimmeler. Is clonal expansion different in older patients? This is another question she finds fascinating. "It might be that clonal expansion is no longer that efficient in older people, which is why a lot of damaged tissue dies off after a heart attack and forms scar tissue which cannot be reactivated through the formation of new blood vessels," says Dimmeler. "If we manage to characterize the clonally expanding cells more precisely, we will hopefully find ways to re-stimulate this process."
Advertisement