A reclassification of obesity is necessary to diagnose obesity-related health risks, as Body Mass Index (BMI) may not be a valid measure for postmenopausal women.

‘Body Mass Index (BMI) is not a valid measure of obesity and there is a need to develop a better measure of obesity for postmenopausal women.’





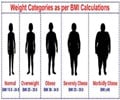
A study published online in Menopause, the journal of The North American Menopause Society (NAMS), demonstrates that the long-accepted BMI definition for obesity may no longer be accurate.Body mass index (BMI) is the most widely used indicator of obesity. Despite its common usage, there is growing concern in the medical community that BMI is not a valid measure of obesity in older adults because it doesn’t account for the location of body tissue used for the storage of fat, differentiate between fat mass and lean mass, or account for variation in body composition. This creates challenges for healthcare providers who must assess obesity-related health risks in their patients.
The challenge is magnified when treating older women because of the significant physical changes that occur during the postmenopausal period, including changes in body weight, redistribution of fat tissue, decrease in skeletal muscle mass, and loss of height.
The location of fat affects a person’s health, even though BMI does not take into account whether a woman has a pear-shaped body with more subcutaneous fat in the hips and thighs or an apple-shaped body consisting of a larger midsection.
Use of BMI in a postmenopausal population where the location of stored fat is changing may result in the misclassification of obesity status and an inaccurate representation of obesity-related risks. There are, however, direct measures of adiposity (fat storage), such as dual-energy x-ray absorptiometry (DXA) scans, that provide a much more accurate measurement of body fat, but these require access to expensive specialized equipment and skilled technicians.
Advertisement
Findings indicate that the use of BMI can lead to bias in measuring the effects of obesity on health outcomes in postmenopausal women. Because women are now expected to spend more than a third of their lives beyond the menopause transition, these findings on the shortcomings of using BMI to define obesity could have serious implications for healthcare providers with an aging patient population.
Advertisement
"Traditional measurement of height and weight may not reflect the degree of obesity for a given woman. Currently, a BMI of 30 kg/m2 is used as a cut-off or measure of obesity for decisions about the degree of surgical risk and in research to determine the effect of obesity on mortality and morbidity. However, BMI may not be a valid measure of obesity for postmenopausal women as they age. A better measure is needed to determine which postmenopausal women meet the definition of obesity for research and clinical care purposes."
Source-Eurekalert