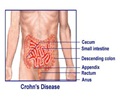
Managing current demand for bowel cancer services has become an increasingly important issue.
Managing current demand for bowel cancer services has become an increasingly important issue with the roll out of Australia’s National Bowel Cancer Screening Program.
Four separate articles in the latest Medical Journal of Australia (MJA) look at various issues related to the implementation of the program.In his editorial for the MJA, Professor Finlay Macrae, Head of Colorectal Medicine and Genetics at Royal Melbourne Hospital, says there are some uncertainties about whether the health system can cope with the extra need for colonoscopies that will be generated by the program.
“It should be possible to spread the load across both private and public facilities, with appropriate jurisdictional contractual agreements between Federal and State Governments, and optimal use of existing facilities and personnel,” says Prof Macrae.
Prof Macrae says it is the responsibility of hospital administrators to identify any funding opportunities for extra services and match resources to the increased demand for services.
A study by Dr Jane Young, Executive Director of the Surgical Outcomes Research Centre at the University of Sydney, and colleagues, on behalf of the Cancer Council NSW shows hospital administrators can also aid uptake of the current guidelines for colorectal cancer treatment and care.
“Our findings show that, on average, 78 per cent of relevant guidelines were followed for individual patients,” says Dr Young.
Advertisement
“The considerable variation found in the application of the National Health and Medical Research Council’s guidelines for colorectal cancer implies that better strategies are needed to ensure greater compliance.”
Advertisement
Dr Viiala suggests reduced waiting times could be achieved by increasing the capacity and productivity of endoscopic units or by ensuring the appropriateness of procedures, for example by stricter adherence to guidelines for surveillance colonoscopies.
“The recognition of risk factors for a diagnosis of cancer, including age over 65 years and certain blood-loss indications, could ensure that most patients with cancer are diagnosed within a three month waiting period,” says Dr Viiala.
Associate Professor Cameron Platell of the School of Surgery and Pathology at the University of Western Australia, and colleagues, conducted a study into survival rates of colorectal cancer patients in public versus private hospitals.
They found patients receiving treatment in a private hospital had improved survival outcomes compared with those treated in public hospitals.
“If these observed improvements are a result of superior treatment, and not just patient selection, then they raise serious concerns regarding equity and access to treatment,” says Assoc Prof Platell.
“The reasons for these improved survival outcomes in private hospitals need to be further elucidated.”
Source-AMA
SRM