Atleast one in 20 patients who undergo surgeries to increase the blood supply to the heart and to stop repeated heart attacks will do better if their hearts are remoulded to the normal size
According to cardiac surgeons at Johns Hopkins atleast one in 20 patients who undergo surgeries to increase the blood supply to the heart and to stop repeated heart attacks will do better if their hearts are remoulded to the normal size, by cutting and suturing together stretched muscle and scar tissue resulting from the initial attack.
In a study to be presented Jan. 28 at the 44th annual meeting of the Society of Thoracic Surgeons in Fort Lauderdale, Fla., the Hopkins team found that by combining so-called coronary artery bypass grafting, known as CABG, with surgical ventricular restoration, or SVR, in patients with advanced heart failure, the likelihood of subsequent heart problems was 24 percent, compared to 55 percent in those undergoing CABG alone.“Cardiologists and cardiac surgeons with patients about to undergo coronary bypass surgery should clearly be considering ventricular restoration,” says senior study investigator and cardiac surgeon John Conte, M.D. A quarter-million Americans undergo bypass surgery each year. “For those who qualify for the dual procedure, the trend is clearly toward living longer, with fewer hospitalizations and improved quality of life.”
Moreover, Conte says, the combined procedure in patients with moderate heart failure offers increased chance to delay or put off entirely the need for a heart transplant. He points out that there is a tremendous shortage of organs available for heart transplantation, with nearly 3,000 Americans currently on waiting lists.
Conte, an associate professor of surgery at the Johns Hopkins University School of Medicine and its Heart Institute, cautions that not all CABG patients can benefit from SVR and that the procedure is most appropriate for those with moderate to severe heart failure, whose pumping function has dropped to less than 35 percent (with 65 percent being normal), and who have suffered a clearly defined heart attack in the heart’s main pumping chamber, the left ventricle. “We estimate that about one in 20 CABG patients who have congestive heart failure are in this category from the volume of patients we see here at Hopkins,” says Conte.
The new study compared results for two groups of men and women at Hopkins, with similar degrees of heart failure and medical histories. One group of 62 had the dual procedure and another group of 58 had CABG only. All were operated on between June 2002 and December 2005 and monitored afterwards by phone and regular check-ups.
The study is believed to be the first head-to-head comparison of the single and dual procedures that applied strict scientific controls, using similar patients in both groups and the same team of surgeons to ensure a uniform quality of surgery.
Advertisement
Death rates during surgery with either CABG alone or CABG with SVR remained the same (at 5.2 percent and 6.4 percent, respectively) and measures of pumping function, called the ejection fraction, also improved by the same amount (at 32 percent and 34 percent.) Researchers plan to continue monitoring the study patients to better assess long-term survival rates.
Advertisement
The add-on procedure, he says, takes a half hour beyond the average two-hour, single CABG surgery, in which arteries from other parts of the body are transplanted to the heart in order to increase its blood supply and to get around, or bypass, arteries narrowed from disease.
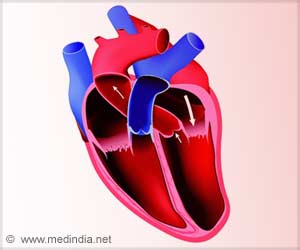
In SVR, surgeons cut open the left ventricle and sew it back together - without actually removing any tissue - to more closely resemble a smaller, normally shaped heart. Often, a patch is sewn over the cut areas to hold the newly shaped heart together.
“Remodeling the heart can restore the heart to its normal, elliptical shape, lowering the pressure buildup inside the heart cavity, reducing the amount of oxygen and energy needed by the muscle to keep pumping, and allowing the heart to work normally.” says Conte, director of heart and lung transplantation at Hopkins.
Both CABG and SVR are covered by Medicare and by most health insurance plans. Costs vary according to how many arteries must be bypassed and what other parts of the organ also need to be shored up. The standard Medicare rate for a single CABG is $1,800, with SVR costing an additional $700.
According to researchers, stretched heart muscle and scar tissue, known as ventricular dilation, is a common consequence of heart attack. The heart dilates, or thins out, in response to increasing pressure within the heart, forcing it to work harder and less efficiently to pump blood through the body. Heart valve leakages commonly result, which may also require surgical repair.
The latest estimates from the American Heart Association, in 2004, show that over 5 million Americans are currently afflicted by heart failure, with nearly three-quarters preceded by high blood pressure. All are at greater risk of hypertrophy and heart attack.
Source-Eurekalert
LIN/K