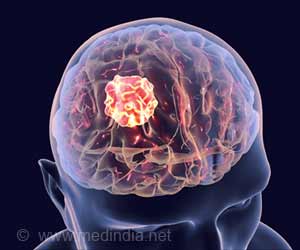
Calcium-sensing receptor, a protein, makes lung cancer deadlier. It could precipitate a syndrome called hypercalcemia, a debilitating disorder.

As these tumors grow, the receptor releases a hormone that sets off a biological cycle that leads to the erosion of bone throughout the body. When the bone breaks down, calcium is released. The excess calcium that can’t be filtered by kidneys cycles back to the receptors, which release more of the damaging hormone. That same hormone promotes the growth and spread of cancer.
Knowing the receptor’s role in squamous-cell lung cancers will help guide future research on new treatment options for both the cancer and hypercalcemia, said Gwendolen Lorch, assistant professor of veterinary clinical sciences at Ohio State University and lead author of the study.
“The calcium-sensing receptor clearly has a huge role in hypercalcemia. Though it’s too soon to say it could be a target for treatment, we won’t ever be able to find the right target if we don’t know how hypercalcemia develops in the first place,” Lorch said.
The researchers also found that lung cancer patients who have a specific type of inherited genetic mutation are at risk of developing hypercalcemia earlier than others. This finding is likely to have clinical implications in the future, as sequencing of the human genome becomes more affordable and available as part of standard medical care, Lorch said.
The research is published in a recent issue of the journal Neoplasia.
Advertisement
Lorch and colleagues obtained squamous-cell lung cancer cell lines from three human patients. The researchers first showed with genetic data that all of these cells had produced proteins that indicated that the cells contained calcium-sensing receptors – a new finding in itself.
Advertisement
“This told us that when people are hypercalcemic, they are producing the maximum level of PTHrP,” Lorch said.
An experiment in mice confirmed the calcium-sensing receptor’s role. Mice were injected with either regular tumor cells or cells from which the calcium-sensing receptor had been stripped away. Mice that received cells without the receptor developed hypercalcemia in 49 days, compared to 29 days for mice that received typical tumor cells, which do have the receptor.
“That’s a very big difference in time in mice,” Lorch said. “This suggests that the calcium-sensing receptor was necessary for the rapid development of hypercalcemia.”
The receptors on those cells also behaved as expected in additional cell line experiments exploring their behavior after the PTHrP hormone was released. All three lines led to the release of what is known as intercellular calcium, but at different levels and rates. One line in particular stood out. This line, called HARA, had previously produced the most PTHrP when stimulated with calcium, and then released much more excess calcium than the other two cell lines.
These findings in the tissue studies led the scientists to sequence the calcium-sensing receptors in the three cell lines to look for genetic variants. The HARA line contained a mutation known as a single nucleotide polymorphism, or SNP (pronounced snip), that influenced how much of the PTHrP protein the receptors produced and how much calcium it took to stimulate that action.
What this means is that lung cancer patients who have two copies of this mutation – one from each parent – are more likely to develop hypercalcemia even before their blood work shows elevated levels of calcium.
“The significance of this is if you have two copies of the mutation, it would be ideal for a clinician to know that you have this mutation and start pre-emptive fluid therapy or other preventive treatment. Even in the normal calcium range, this mutation is going to set a person up for hypercalcemia much earlier than other patients,” Lorch said.
Source-Medindia