More than 85% of Canadian provinces and territories restrict access to new direct-acting antivirals (DAA) for the treatment of hepatitis C.

‘The only way to eliminate hepatitis C is by adopting a national strategies and goals to screen and treat all infected individuals using antivirals by negotiating the cost with pharmaceutical companies.’





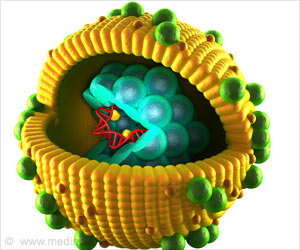
More than 220,000 people in Canada are infected by the Hepatitis C virus. The disease is transmitted by blood. One person in four spontaneously clears the virus before it attacks the liver. The rest often don not feel any symptoms at the beginning, but gradually develop liver disease, graded from F0 to F4. F0 corresponds to the initial infection without fibrosis and F4, to cirrhosis.A study conducted by researchers at the University of Montreal Hospital Research Centre (CRCHUM), The Kirby Institute, UNSW Australia, and the Canadian Network on Hepatitis C (CanHepC) shows that nearly everywhere in Canada, provinces and territories impose obstacles to the reimbursement of these medications by the public system because of their cost.
It imposes all types of conditions before reimbursing any of the direct-acting antivirals: a fibrosis level of F2, prescription from a specialist physician, the absence of HIV infection, etc.
"There are many new direct-acting antivirals, marketed by different pharmaceutical companies. We studied reimbursement practices for simeprevir, sofosbuvir, ledipasvir-sofosbuvir and paritaprevir-ritonavir-ombitasvir plus dasabuvir. We found that 85 to 92% of the provinces and territories in Canada restrict access to these medications to persons with moderate fibrosis," affirmed Alison Marshall from the Kirby Institute, UNSW Australia, lead author of a study to appear in CMAJ Open.
"The treatment is effective, safe and economically viable. We should treat all people infected with hepatitis C," insisted Dr. Julie Bruneau, a physician and researcher at the CHUM. Canada is committed to the World Health Organization's objective of eradicating hepatitis by 2030.
Advertisement
If the trend continues, the costs associated with treating patients with cirrhosis of the liver will increase from $161M to $258M a year in 2035.
Advertisement
Scientists at the Canadian Network on Hepatitis C are calling for a national strategy to eliminate hepatitis C in the country. "Even though health care is the responsibility of the provinces and we have 13 public health insurance plans in Canada, we need a national plan and shared goals that can be adapted to local realities. We did it for HIV and we should also do it for hepatitis C," argues Naglaa Shoukry, a researcher at the CRCHUM and the director of the Canadian Network on Hepatitis C.
In Australia, this type of approach provided leverage to negotiate the price of antivirals with pharmaceutical companies, enabling access to HCV therapy for all patients living with hepatitis C with no restrictions based on severity of liver disease. In the first five months of therapy being available, 26,500 have received treatment (12% of the estimated total with chronic hepatitis C).
"At the present time in Canada, it's the law of supply and demand; there are negotiations on a company-by-company, pill-by-pill basis. There is no transparency and we don't really know how much the new antivirals really cost. The only way to eliminate hepatitis C is by adopting a national strategy to screen and treat all infected individuals, particularly people who inject drugs," concluded Naglaa Shoukry.
Source-Medindia