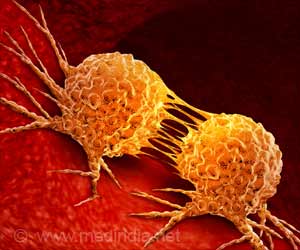
A naturally occurring protein used to treat cancers has been modified to boost potency and reduce toxicity, say scientists.

But a Stanford University School of Medicine scientist has generated a mutant version of the protein whose modified shape renders it substantially more potent than the natural protein while reducing its toxicity.
IL-2 is a master regulator of the immune system. It acts as a growth factor for many different kinds of immune cells, including an all-important class called T cells. These cells can both recognize and organize attacks against pathogens or tumors.
The protein stimulates T cells' proliferation in response to these threats. That makes it a potent anti-cancer drug. When injected into a patient, it spurs fierce anti-tumor activity.
"In a substantial subset - about 7 percent - of patients with advanced metastatic melanomas or kidney cancers, IL-2 treatment actually cures the disease," said Christopher Garcia, professor of molecular and cellular physiology and of structural biology, and the study's senior author.
That's an impressive result, considering the failure of most treatments at such a late stage of cancer.
Advertisement
This in turn is the result of leakage from the copious capillaries that permeate lung tissue, the better to carry away oxygenated blood to distant tissues.
Advertisement
For this study, Garcia's group produced a vast variety of mutated versions of the protein, and then, in a test-tube competition, compared the strength of these mutant proteins' binding to a particular cell-surface receptor, a process that is crucial to the T-cell activation needed to treat cancer.
The researchers eventually obtained a mutant that Garcia dubbed "Super-2," which had more than 300 times the receptor-binding strength of natural IL-2. In subsequent tests designed to assess Super-2's ability to impede tumor growth, the new molecule outperformed natural IL-2 by a significant margin.
The researchers also tested Super-2 to determine the extent of the side effects it would cause. To do this, they collaborated with a co-author of the study, Onur Boyman, MD, of University Hospital Zurich in Switzerland, who had previously found that the type of cells in the lung that are responsible for capillary leakage have receptors for IL-2.
Boyman developed an assay for IL-2's most dose-limiting side effect, pulmonary edema. This assay compares the weight of lungs from mice treated with a test compound versus lungs that are not thusly treated. The greater the weight difference, the more fluid build-up has occurred.
Boyman and a member of his group, Carsten Krieg, PhD, carried out all the animal research used for the study. By this assay, pulmonary edema caused by Super-2 was significantly and substantially less than by natural IL-2.
What makes Super-2 so effective, said Garcia, is its altered shape. A T-cell's IL-2 receptor complex consists of three separate protein components sitting on the cell's surface.
But the mutations Garcia's team induced lock Super-2 into a configuration whose optimized shape lets it bind directly to beta, bypassing alpha. The three-dimensional structure of Super-2, together with computer simulations from the laboratory of associate professor of chemistry Vijay Pande, PhD, suggested this was because the mutant form of IL-2 was less "floppy" than the natural form, so that it presented a "tighter" binding surface to the beta receptor.
This souped-up form of the protein was several times as potent as the naturally occurring form of IL-2 at slowing tumor growth, as measured by assays employing three different tumor types in culture.
Major pharmaceutical companies have expressed an interest in Super-2, according to Garcia, who said he suspects that a licensing agreement from one of them may be in the offing. Stanford has applied for a patent on Super-2.
However, he said, a group at the National Institutes of Health, including some of the heavyweight scientific experts who originally put IL-2 through its clinical paces some years ago, is now testing Super-2 from Garcia's lab in a large number of tumor models, in the hope of fast-tracking its development as a new therapy for additional cancer indications.
"I hope it goes this route, because that would mean human trials would get started more quickly," Garcia said.
The findings appeared online in Nature.
Source-ANI