Benefits of therapeutic hypothermia is similar in cardiac arrest patients with preexisting enlarged hearts or cardiomyopathy, compared with those patients without cardiomyopathy.

"While it is well established that therapeutic hypothermia is neuroprotective and increases survival in resuscitated cardiac arrest patients without cardiomyopathy, we sought to determine whether catastrophic outcomes in cardiac arrest patients with preexisting cardiomyopathy are avoidable," said Michael R. Mooney, MD, a cardiologist at the Minneapolis Heart Institute® at Abbott Northwestern Hospital in Minneapolis and physician researcher with Minneapolis Heart Institute Foundation.
From February 2006 to July 2010, Mooney and his colleagues enrolled 192 consecutive cardiac arrest patients who remained unresponsive following return of spontaneous circulation in a therapeutic hypothermia protocol, regardless of initial rhythm, hemodynamic status or prior medical history. They hypothesized that there would be a high prevalence of preexisting cardiomyopathy in this patient population, and therapeutic hypothermia would confer similar neurologic and survival benefit compared to non-cardiomyopathy patients.
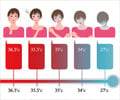
Of the 192 patients, 43.8 percent had preexisting cardiomyopathy, of which ischemic was the most common type (41.7 percent). Patients with preexisting cardiomyopathy were older (65.7 years vs. 61.7 years) and more likely to be male (83.3 vs. 63.9 percent).
The majority presented in ventricular fibrillation/ventricular tachycardia (75 percent and 70.4 percent) in both the cardiomyopathy and non-cardiomyopathy groups. There was a higher prevalence of concurrent STEMI in the cardiomyopathy group (27 vs. 18.5 percent), which was not statistically significantly. Cardiogenic shock was more prevalent in the cardiomyopathy group (54.8 vs. 28.7 percent).
While the cardiomyopathy groups were slightly higher, the survival between the two groups (52.4 vs. 51.9 percent) and survival with favorable neurologic outcome, defined by Cerebral Performance Category 1 or 2, (46.4 vs. 49.1 percent), were similar. They found that survival with favorable neurologic outcome in cardiomyopathy patients with cardiogenic shock was 34.8 percent, compared with 45.2 percent in non-cardiomyopathy cardiogenic shock patients.
Advertisement
Advertisement