Mitochondria play a central role in maintaining optimal cardiac performance and deregulated mitochondrial activity plays a causative role in heart diseases.
‘Myocardium, the muscular wall of the heart, is a high-energy-demand tissue and, mitochondria play a central role in maintaining optimal cardiac performance.’





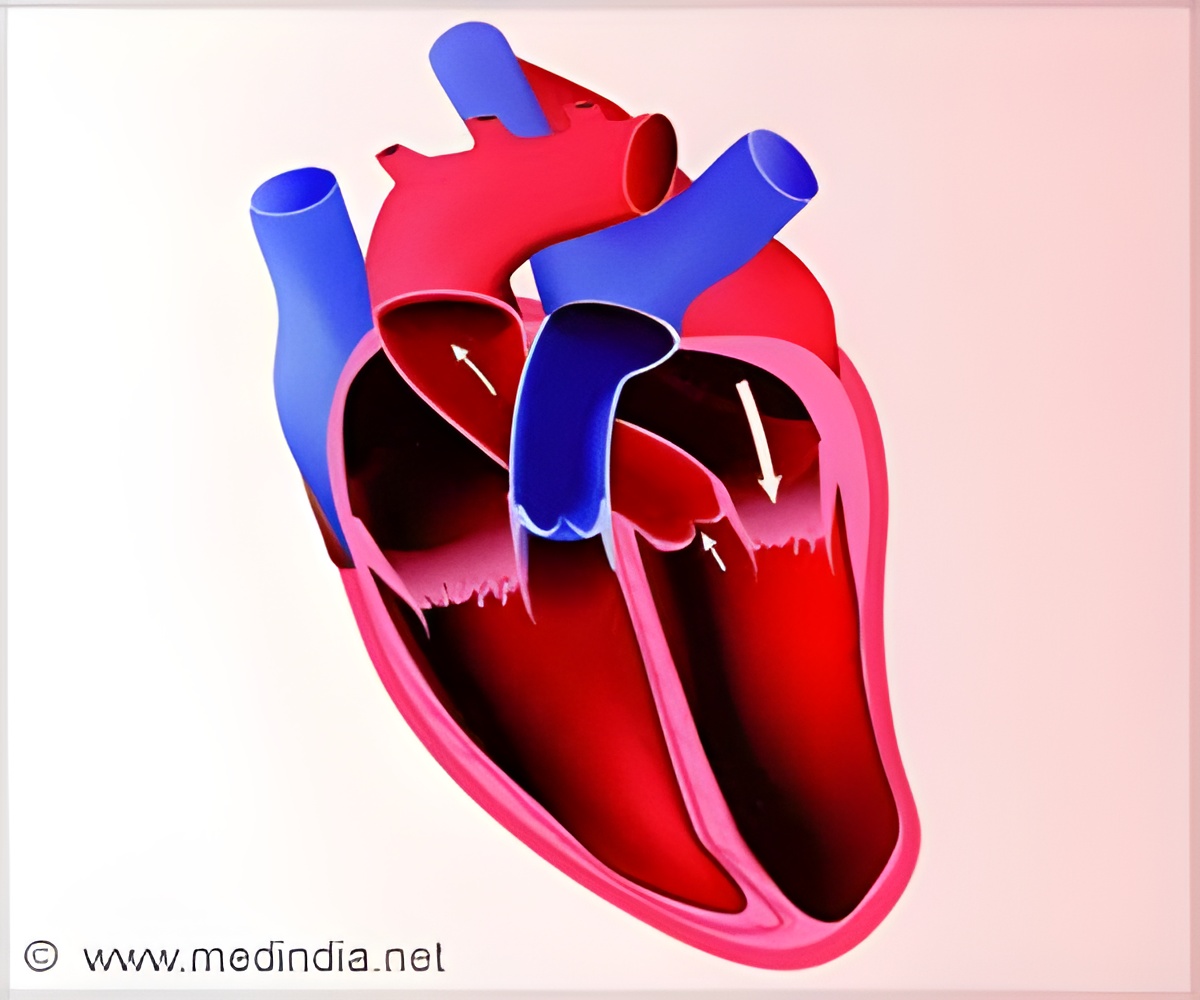
Also, disrupting how FUNDC1 binds to a particular receptor inhibited the release of calcium from another cell structure, the endoplasmic reticulum (ER), into the mitochondria of these cells and resulted in mitochondrial dysfunction, cardiac dysfunction and heart failure. The findings are published in the journal Circulation. Mitochondria play numerous roles in the body, including energy production, reactive oxygen species generation and signal transduction. Because the myocardium, the muscular wall of the heart, is a high-energy-demand tissue, mitochondria play a central role in maintaining optimal cardiac performance. Growing evidence suggests deregulated mitochondrial activity plays a causative role in cardiovascular diseases.
In the body, mitochondria and ER are interconnected and form their own endomembrane networks. The points where mitochondria and ER make physical contact and communicate are known as mitochondria-associated ER membranes (MAMs). MAMs play a major role in regulating the transfer of calcium between ER and mitochondria. Dysfunctional MAMs are involved in several neuronal disorders, including Alzheimer’s disease and Parkinson’s disease. Until now, the role of MAMs in cardiac pathologies has not been well understood.
"Our study found the formation of MAMs mediated by the mitochondrial membrane protein FUNDC1 was significantly suppressed in patients with heart failure, which provides evidence that FUNDC1 and MAMs actively participate in the development of heart failure," said Dr. Ming-Hui Zou, director of the Center for Molecular and Translational Medicine at Georgia State and a Georgia Research Alliance Eminent Scholar in Molecular Medicine. "This work has important clinical implications and provides support that restoring proper function of MAMs may be a novel target for treating heart failure."
The researchers used mouse neonatal cardiomyocytes, mice with a genetic deletion of the FUNDC1 gene, control mice with no genetic deficiencies and the cardiac tissues of patients with heart failure.
Advertisement
To determine if FUNDC1 reduction occurred in human hearts and contributed to heart failure in patients, the researchers examined four heart specimens from heart failure patients and four heart specimens from control donors. They found the levels of FUNDC1 were significantly reduced in patients with heart failure compared to control donors. Also, the contact between ER and mitochondria in failed hearts was significantly reduced. In addition, the mitochondria in heart failure hearts were more elongated compared to those in control donors.
Advertisement