A survey based on the 30-day outcome of 1,450 CAS patients and 1,368 CEA patients revealed that CEA yields better short-term results than CAS in patients with carotid artery disease.
According to a 30-day outcomes report from the Society for Vascular Surgery (SVS) Vascular Registry for Carotid Procedures, Carotid endarterectomy (CEA) yields better short-term results than carotid artery stenting (CAS) in patients with carotid artery disease.
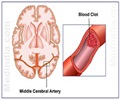
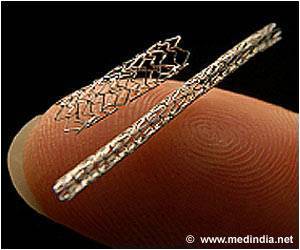
Carotid artery disease is marked by stenosis (narrowing) of the carotid artery, located on either side of the neck, which supplies blood to the brain. Typically, this has been treated by performing an open repair surgery (CEA).An endovascular procedure (CAS) treats patients who are at risk for complications such as prior carotid artery surgery (i.e., CEA), neurological conditions (i.e., prior stroke), or exposure to radiation at the neck.
The SVS Outcomes Committee developed the Vascular Registry for Carotid Procedures in response to the 2005 Centers for Medicare and Medicaid Services National Coverage Decision on carotid artery stenting.
The SVS Vascular Registry went live on July 2005, as the first societal registry to enroll CAS and CEA patients. Data are allocated to visit intervals of 30-day, six-month, one-year, and subsequent annual evaluations.
“As of December 26, 2007, 6,403 procedures with discharge data were entered by 287 providers at 56 centers,” said Flora Siami, MPH, director, regulatory affairs and principal research scientist at New England Research Institutes, Inc. in Watertown, Mass. “In addition there were 1,450 CAS patients and 1,368 CEA patients with 30-day outcomes.”
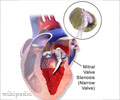
“Our primary outcome of interest was combined death, stroke, and myocardial infarction at 30-days post-procedure,” said senior author Anton Sidawy, MD, MPH, FACS, chief of vascular surgery at Veterans Affair Medical Center in Washington, D.C. and professor of surgery at both Georgetown and George Washington University Schools of Medicine, in Washington, D.C. “The SVS Outcomes Committee also reviewed demographics, comorbidities, intra-operative complications.”
“In general, there was a greater proportion of CAS patients with pre-procedure lateralizing neurological symptoms, as well as higher prevalence of cardiac comorbidities compared with CEA patients.”
When CAS and CEA were compared in the treatment of atherosclerotic disease only, the difference in outcomes between the two procedures was more pronounced, with death/stroke/MI 6.42 percent after CAS vs. 2.62 percent following CEA, p<0.0001. Thus, following best possible risk adjustment of these unmatched groups, symptomatic and asymptomatic CAS patients had significantly higher 30-days post-procedure incidence of death/stroke/myocardial infarction when compared to CEA patients.
Dr. Sidawy explained, “Given the trend observed in the Vascular Registry, there is no justification to expand the use of CAS until the results of the randomized CREST trial are published providing level one evidence.”
“This initial report from the Vascular Registry provides proof of concept that a specialty society-based vascular registry can succeed in meeting regulatory and scientific goals,” said Gregorio Sicard, MD, chair, SVS Outcomes Committee, and chief of vascular surgery and professor of surgery at Washington University in St. Louis. “With continued enrollment and follow-up, analysis of SVS Vascular Registry will supplement randomized trials by providing real-world comparisons of CAS and CEA with sufficient numbers to serve as an outcome assessment tool of important patient subsets and across the spectrum of peripheral vascular procedures.”
The SVS Vascular Registry for Carotid Procedures currently has 77 participating clinical facilities and over 9,700 patients. The SVS Vascular Registry provides semi-annual institutional benchmarking reports to participating facilities on outcomes by procedure.
New England Research Institutes, Inc. serves as the independent data coordinating center, maintaining the database and performing statistical analysis. The SVS designed the Vascular Registry with potential for expansion to procedures involving other vascular beds.
This is published in the January 2009 issue of the Journal of Vascular Surgery, by the Society for Vascular Surgery.
Source-Newswise
PRI/SK
 MEDINDIA
MEDINDIA



 Email
Email