Patients who receive more cells during cell therapy for heart attacks get significant benefits, a new study has suggested.
Study's principal investigator, Arshed Quyyumi, MD, professor of medicine at Emory University School of Medicine and co-director of the Emory Clinical Cardiovascular Research Institute, said that this was an enormous undertaking, one that broke new ground in terms of assessing cell therapy rigorously and they made some real progress in determining the cell type and doses that can benefit patients, in a group for whom the risks of progression to heart failure are high.
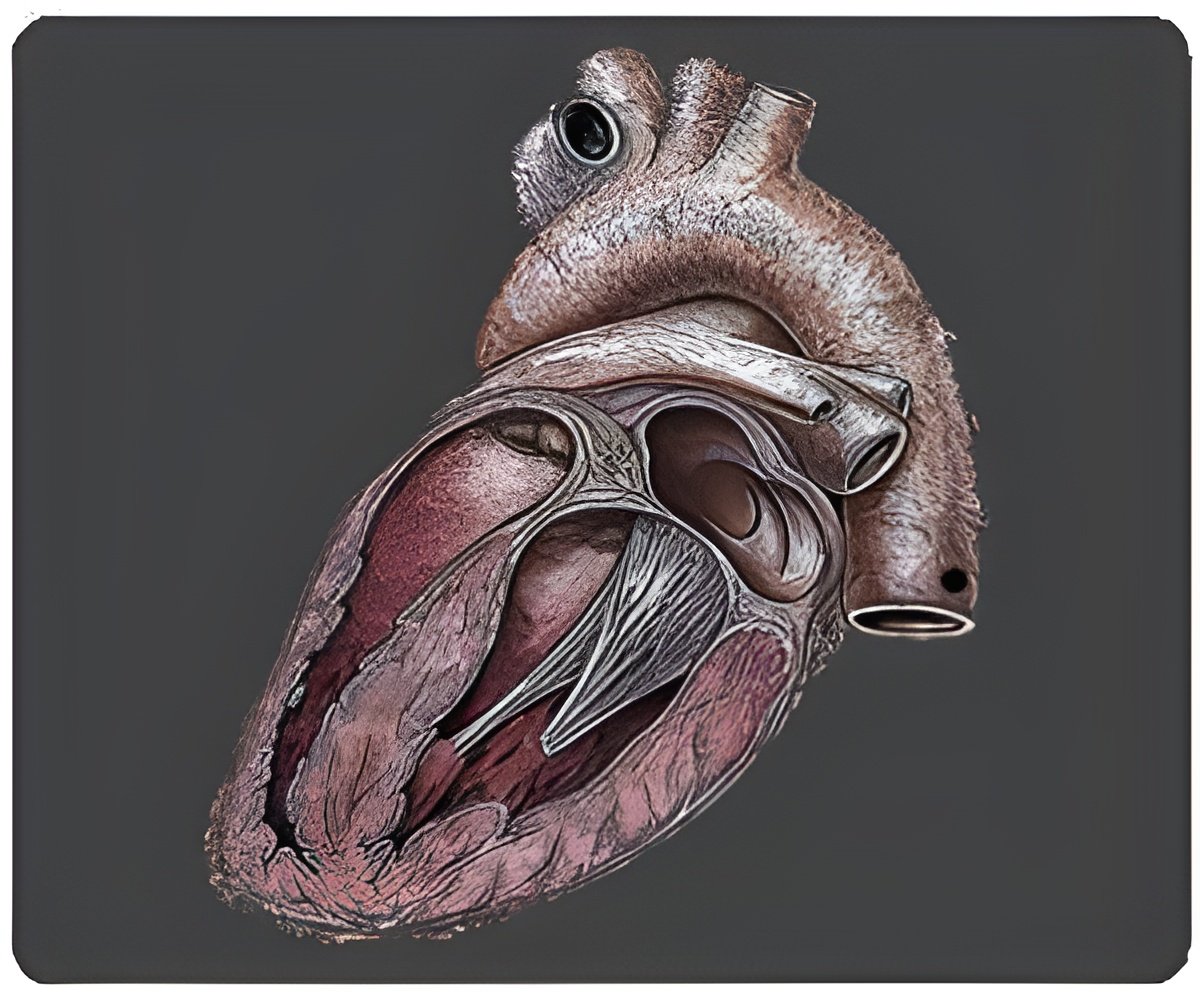
All participating patients received the standard of care-stent placement-and were only enrolled if, four days after heart attack and stenting, their ejection fraction (a measure of the heart's pumping capacity) was less than 48 percent. The average starting ejection fraction was 34 percent, a sign of severe injury to the heart. After enrollment, patients had cells extracted from their bone marrow and received an intracoronary injection of sorted bone marrow cells or a placebo. Not all patients received the same dose of cells. Patients were supposed to receive a minimum of 10 million cells but some received more, up to 40 million.
Recovery and outcomes were assessed in several ways: MACE (major adverse cardiac events, ranging from hospitalization for chest pain to death), ejection fraction, measured by magnetic resonance imaging, and perfusion or blood flow in the heart, measured by SPECT imaging. Cardiac imaging was performed six months after treatment, and MACE came from an average of twelve months of follow-up.
MACE occurred in 14 percent of control patients, in 17 percent of those of who received less than 14 million cells, in 10 percent of those who received greater than 14 million cells, and in 7 percent of those who received greater than 20 million cells. Mortality was 3.6 percent in the control group, and zero in the entire treatment group.
Displaying a similar dose-dependent trend, starting from an average of 34 percent, ejection fraction increased 4.9 percent in controls, 3.1 percent in the group receiving less than 14 million cells, 5.8 percent in the group receiving more than 14 million cells, and 10.2 percent in the group receiving more than 20 million cells. There were no significant effects on improvement in blood flow in the heart, as measured by SPECT imaging.
Advertisement
Source-ANI