Many stroke patients who receive prompt hospital treatment with clot-busting tissue plasminogen activator (tPA) therapy can avoid lengthy stay in ICU.

Results show that a relatively simple measure of stroke severity can accurately single out which patients need ICU monitoring and which can be managed outside of a critical care setting in the hospital.
"What we saw in this preliminary study was that, after the initial hour-long infusion of tPA, if an intensive care need had not developed, the chance of needing ICU monitoring - including a symptomatic 'bleed' - was extremely low for a large majority of patients, namely those with milder strokes," says Victor Urrutia, M.D., medical director of the Comprehensive Stroke Center at The Johns Hopkins Hospital and head of the research team.
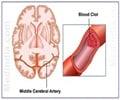
Ischemic stroke, caused by a clot in a blood vessel that cuts off blood flow to the brain, is the most common form of stroke and the second leading cause of death for those over 60. In the United States, an estimated 795,000 people suffer a stroke each year. So far, tPA is the only FDA-approved treatment for acute stroke.
In a report on the study published online in the journal PLOS ONE, the Johns Hopkins team analyzed data from 153 stroke patients admitted to the emergency departments of The Johns Hopkins Hospital and Johns Hopkins Bayview Medical Center between 2010 and 2013. After taking into account differences in age, sex, race, hypertension, diabetes, atrial fibrillation, kidney function, blood clotting status, use of statin drugs and other health factors, the team says that what emerged as the best predictor of the need for intensive care was a patient's score on the National Institutes of Health (NIH) Stroke Scale, a trusted measure of stroke severity. The scale is a proven tool administered at the bedside involving 15 measures and observations, including level of consciousness, language ability, eye movements, vision strength, coordination and sensory loss. Scores range from zero to 42, with mild strokes typically registering 10 or lower. The average score for the Johns Hopkins patient group was 9.8.
"What we learned is that the majority of our patients with mild strokes required no critical care, and that we are using scarce, specialized resources for intensive monitoring rather than for intensive care," says Urrutia, an assistant professor of neurology.
Advertisement
Urrutia emphasized that critical care is clearly needed for tPa-linked bleeding, stroke-related brain swelling and critical abnormalities in blood pressure or blood sugar.
Advertisement
In the follow-up study, which is scheduled to begin this spring, consenting patients with a low stroke scale score and no other apparent need for intensive care will enter a stroke unit with a less rigorous monitoring schedule and increased family visiting time.
Patients in the non-ICU setting will be less physically restricted and subjected to fewer sleep interruptions, lowering the risk of ICU-associated delirium and psychological distress. "We expect benefits to extend to the hospital as well, freeing up the ICU staff and beds for sicker patients," says Urrutia.
The financial benefits of the change in protocol could be significant, Urrutia adds. "Present monitoring for patients with tPA is very costly," he says.
Source-Eurekalert