When patients with drug-resistant bacteria are admitted to hospitals without showing symptoms caused by the bacteria, there is a potential for spread to others.
‘A better understanding of how multi drug-resistant bacteria is transmitted between hospitals and nursing homes will enable us to develop control strategies.’





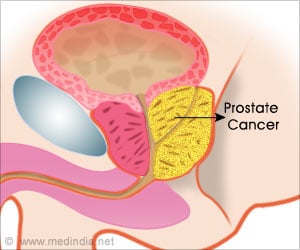
"When patients with drug-resistant bacteria are admitted to hospitals, there is a potential for spread to others," said Leonard Mermel, D.O. ScM, medical director of the epidemiology and infection control department at Rhode Island Hospital and author of the study. "A better understanding of how such bacteria is transmitted between hospitals and nursing homes will enable us to develop control strategies." Mermel and colleagues documented patients admitted to Rhode Island Hospital and The Miriam Hospital from area nursing homes in 2012. They screened these patients for the presence of carbapenem-resistant Enterobacteriaceae (CRE) since there is little data in the medical literature regarding how prevalent these drug-resistant bacteria are among asymptomatic nursing home patients at the time of admission to hospitals.
The researchers identified highly resistant bacteria in 23 of the 500 acute care hospital admissions from the nursing homes, seven of these were carbapenem-resistant Enterobacteriaceae. They found that the use of a feeding tube was associated with gastrointestinal carriage of these bacteria.
"Such information is helpful in better understanding transmission of such resistant bacteria between nursing homes and hospitals, helpful to focus efforts to reduce antibiotic pressure in nursing home settings, and to better assess the risks and benefits of feeding tubes in this patient population," said Steven Kassakian, M.D., a study co-investigator and a post-doctoral fellow in clinical informatics at Oregon Health and Science University.
Cheston Cunha, M.D., one of the study's co-investigators and director of the antibiotic stewardship program at Rhode Island Hospital and the Miriam Hospital, added, "Antibiotic resistance has been called one of the world's most pressing public health problems. When antibiotics fail, infections often last longer, cause more severe illness, require more doctor visits or extended hospital stays, and involve more expensive and toxic medications. Some resistant infections can even cause death. Because therapeutic options are few if infections occur with antibiotic resistant bacteria, antibiotic stewardship and infection control measures are necessary in limiting the spread of these organisms in healthcare settings."
Advertisement